 |
 |
|
|
Abstract
The central venous cannulation is commonly performed in the operating rooms and intensive care units for various purposes. Although the central venous catheter (CVC) is used in many ways, the malpositioning of the CVC is often associated with serious complications. We report a case of an unexpected malposition of a CVC in the jugular venous arch via external jugular vein.
The central venous catheterization is a simple, relatively inexpensive method of assessing a patient's circulating blood volume, cardiac status, and vasomotor tone, and it is an essential component of modern-day critical care [1]. The most common routes of insertion include the internal jugular, external jugular, subclavian, basilic, and femoral veins via a percutaneous approach [2]. The optimal location of a central venous catheter (CVC) is within the long axis of the superior vena cava (SVC) outside of the right atrium [3]. The misplacement of the CVC inserted via the subclavian, internal jugular, or other veins is not unusual and is the cause of relatively common complications [4]. The CVC positioned incorrectly, whether inside of a vessel other than the SVC or impinging on the wall of the SVC, may cause serious complications [5]. We present a case of malpositioning of a CVC into a jugular venous arch (JVA), which was accidently found in the process of sternotomy during coronary artery bypass graft (CABG) surgery.
A 55-year-old male (weight, 68 kg; height, 170 cm) with three-vessel coronary artery occlusive disease was scheduled for CABG. The preoperative echocardiography revealed a left ventricular ejection fraction of 42% with no other intracardiac pathologies. The coronary angiography also revealed 100% stenosis in the left anterior descending artery, 80% stenosis in the left circumflex artery, and 90% stenosis in the right coronary artery. There was no abnormal laboratory finding.
The patient was premedicated with 1 mg midazolam intravenously and 5.5 mg morphine intramuscularly. In the operating room, initial blood pressure was 128/78 mmHg, heart rate was 95 beats/min, and peripheral oxygen saturation was 100% with oxygen 3 L/min via nasal cannula. The right radial artery was cannulated for continuous monitoring of arterial pressure. The right internal jugular vein (IJV) cannulation was performed and Swan-Ganz catheter was inserted through the sheath introducer. The anesthesia was induced via 2 mg midazolam, sufentanil 50 µg, and vecuromium 8 mg intravenously. While monitoring the blood pressure and cardiac output, trachea was intubated and the lungs were mechanically ventilated with O2, air, and desflurane.
The patient was tilted to 20 degrees Trendelenberg position, and his head was turned 30 degrees rightward. After puncturing the left external jugular vein (EJV) with 18 gauge 2 inch thin-walled needle, the J-tipped guidewire was inserted with Seldinger technique. With this approach, a resistance of guidewire advancement was met at a depth of 9 cm, but it was advanced further without any resistance. A 7-French double lumen central catheter was inserted through the guidewire, and the catheter was fixed at 15 cm mark at the skin level, after free aspiration of venous blood.
After the operation was initiated through median sternotomy, the mid-portion of the CVC which was inserted via left EJV was found in the operation field. The catheter was located in the vein other than the brachiocephalic vein (BV), and the BV was found at about 3 cm below the catheter. There was a small laceration on the vein, and the vein showed continuity with the catheter inside (Fig. 1). There was only a small amount of bleeding around the vessel, because the diameter of the vessel was similar to that of the catheter. We decided not to ligate the vessel immediately due to the possibility of bleeding, so we checked the catheter after the operation. The vein was cut into two parts and was connected to each other with the catheter (Fig. 2). The surgeon ligated the vessel while removing the catheter and the surgery was completed.
The correct placement of the CVC is important in obtaining the accurate central venous pressure (CVP) measurements and hemodynamic management. The inaccurate CVP measurements or inability to obtain an ideal wave from tracing are suggestive of an incorrect location of the catheter tip [6]. The difficulty in inserting or advancing the guidewire should have created an index of suspicion for misplacement of the CVC [3]. In our case, the resistance was encountered during the insertion of the guidewire, and the resistance soon disappeared and the guidewire was advanced further without any other resistance. Also, the venous blood was aspirated freely through each lumen of the CVC. However, the ability to aspirate blood freely from the catheter lumen after the placement of the catheter does not necessarily confirm a proper placement of the catheter tip [7]. Occasionally, despite the proper technique, the tip of the catheter may not terminate at the desired level [8]. The malpositioning of the catheter tip may occur at the time of the insertion or later on as a result of spontaneous migration due to anatomic positioning or pressure changes within the thoracic cavity [9]. Therefore, the routine use of chest radiographs to establish the correct placement of CVC is recommended [7].
For central venous catheterization, Belani et al. [10] found that the IJV route is a more predictable and reliable method but is associated with greater incidence of complications than the EJV route. The EJV route appears to be safer, but has a lower predictability and a higher incidence of catheter malposition. In this case, left EJV was catheterized for the injection of intravenous medications.
At first, it was difficult to identify the exact location of the CVC exposed on the surgical field. The BV was confirmed 3 cm below the catheter in the surgical field. After considerable discussion of the anatomy, we were able to conclude that the CVC was in the JVA.
There are many variations in the venous anatomy of the head and neck between the right and left sides, as well as between individuals [11]. The venous drainage of the head and neck is composed of a deep and a superficial jugular system. The superficial system includes the EJV and the anterior jugular vein (AJV) which originates from the median superficial cervical region. The AJV almost always have an anastomosis with the EJV, and the trunk of the AJV ends in the EJV (46%) or in the subclavian vein (54%). When the AJV ends in the EJV, these vessels form two types of curve: inferior concave (39%) or superior concave (61%) [12]. Just above the sternum, the right and the left AJVs communicate by a transverse trunk, the JVA, which traverses the midline of the neck (Fig. 2) [13].
This collateral venous network at the head and neck can cause malposition of the CVC catheter, especially when the catheter enters the horizontal component of the anterior jugular venous system via the EJV [13]. According to a cadaveric study, a catheterization of the EJV was impossible in 5.6% of the cases, because the EJV was too small; and the catheter ended up in the AJV in 28% of the cases where the catheterization was possible [12]. Furthermore, the inability to identify the vein in obese and short necked patients, not being able to pass the guidewire into the intrathoracic portion of the vein, and failure to pass the catheter can all cause the non-passage of the catheter via EJV [14].
Due to the anatomical variation and complicated venous network, the malpositioning of the CVC into the JVA via EJV is not an uncommon event. But placing a catheter tip in the vessels with small diameter significantly increases the risk of thrombosis, perforation of the vessel, and extravasation of the infusate [15]. In this case, the vessel was damaged by the catheter. The loss of continuity of the vessel seemed to be due to the application of sternal retractor to spread the sternum. If it was removed without ligating the vessel, a serious complication from bleeding could have happened. Since chest X-ray or contrast was not used to confirm the exact anatomy of the vessels in this case, we can presume the horizontal and superior concave curve of the AJV in the EJV (Fig. 3). Therefore, one must always consider the possibility of misplacement of the CVC by checking the central venous wave form and obtaining chest X-ray.
The misplacement of the CVC catheter via the EJV could occur due to anatomical variation and complex venous network. Therefore, one must always consider the possibility of incorrect placement of the catheter. Monitoring the central venous wave form and taking chest X-ray can be useful ways to confirm the position of the catheter.
References
1. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003; 348: 1123-1133. PMID: 12646670.


2. Seneff MG. Central venous catheterization: a comprehensive review-part II. J Intensive Care Med 1987; 2: 218-232.

3. Schummer W, Schummer C. Central venous catheter malposition in the azygos arch. Eur J Anaesthesiol 2002; 19: 832-834. PMID: 12442935.


4. Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization. Failure and complication rates by three percutaneous approaches. Arch Intern Med 1986; 146: 259-261. PMID: 3947185.


5. Gentili DR, Onofrey D, Gabrielson GV, Benjamin E, Iberti TJ. Malposition of central venous catheters outside the central circulation. J Cardiothorac Anesth 1989; 3: 752-756. PMID: 2521035.


6. Agrawal P, Gupta B, D'souza N. Coiled central venous catheter in superior vena cava. Indian J Anaesth 2010; 54: 351-352. PMID: 20882184.



7. Ghatak T, Azim A, Baronia AK, Muzaffar SN. Malposition of central venous catheter in a small tributary of left brachiocephalic vein. J Emerg Trauma Shock 2011; 4: 523-525. PMID: 22090752.



8. Asudani D, Wretzel S, Patel R, Stayman A. The Clinical Picture: A judgment call. Cleveland Clin J Med 2008; 75: 690-695.

9. Rasuli P, Hammond DI, Peterkin IR. Spontaneous intrajugular migration of long term central venous access catheters. Radiology 1992; 182: 822-824. PMID: 1535901.


10. Belani KG, Buckley JJ, Gordon JR, Castaneda W. Percutaneous cervical central venous line placement: a comparison of the internal and external jugular vein routes. Anesth Analg 1980; 59: 40-44. PMID: 6985778.

11. Williams DW 3rd. An imager's guide to normal neck anatomy. Semin Ultrasound CT MR 1997; 18: 157-181. PMID: 9253082.


12. Deslaugiers B, Vaysse P, Combes JM, Guitard J, Moscovici J, Visentin M, et al. Contribution to the study of the tributaries and the termination of the external jugular vein. Surg Radiol Anat 1994; 16: 173-177. PMID: 7940081.


13. Chasen MH, Charnsangavej C. Venous chest anatomy: clinical implications. Eur J Radiol 1998; 27: 2-14. PMID: 9587764.


14. Chakravarthy M, Krishnamoorthy J, Nallam J, Kolur N, Faris A, Reddy K, et al. External Jugular Venous Route for Central Venous Access: Our Experience in 563 Surgical Patients. J Anesthe Clinic Res 2011; 2: 144.

15. Polderman KH, Girbes AJ. Central venous catheter use. Part I: Mechanical complications. Intensive Care Med 2002; 28: 1-17. PMID: 11818994.


Fig. 1
Open chest via median sternotomy. The central venous catheter is visible inside the vein (white arrow). There is a small laceration on the vein.
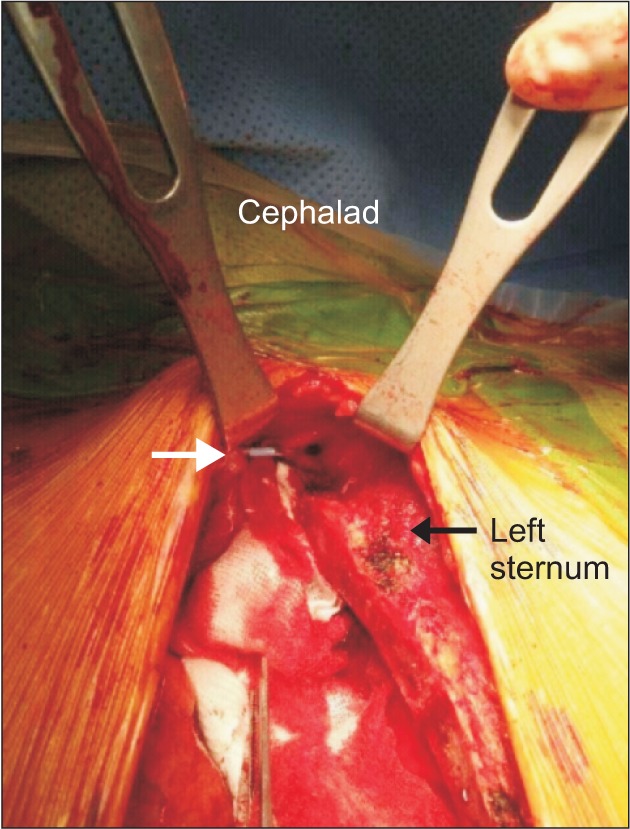
Fig. 2
The catheter was checked at the end of the operation. The vein was cut into two parts and was connected to each other with the catheter (black arrow).

Fig. 3
Schematic diagram of a jugular venous system in the neck. Superior concave end of anterior jugular vein in external jugular vein (arrowhead) and the probable position of central venous catheter (dotted line). AJV: anterior jugular vein, BV: brachiocephalic vein, CVC: central venous catheter, EJV: external jugular vein, IJV: internal jugular vein, JVA: jugular venous arch, SV: subclavian vein, SVC: superior vena cava.

- TOOLS








