|
 |
| Korean J Anesthesiol > Volume 77(1); 2024 > Article |
|
Recommendations for airway management have increasingly focused on the maintenance of oxygenation during airway instrumentation [1,2]. Facemask ventilation (FMV) plays a key role as a method of both routine and rescue ventilation in anesthesiology [1,2] and critical care settings.
Various difficult airway management guidelines include FMV as a relevant item and emphasize its role in hypoxemia or other high-risk situations, including preoxygenation when airway access is challenging for physiological reasons. However, in-depth instructions on how to perform this technique properly or which maneuvers or adjuvant tools can be applied for optimization are not provided. Recommendations provided by the Difficult Airway Society (DAS) emphasize the importance of muscle relaxation (MR) for facilitating FMV and other airway-related maneuvers [1]. Additionally, the American Society of Anesthesiologists (ASA) recommendations highlight the importance of documenting the nature of difficulties in airway management to guide future care delivery [2]. Other guidelines for the management of tracheal intubation in critically ill adults also suggest MR be used for facilitating FMV.
No scales or individual risk factor have been shown to have sufficiently reliable capacity to predict difficult FMV, either alone or in combination [4]. However, routine clinical practice still relies on the global assessment of risk factors rather than the use of a specific tool (such as the Mallampati score for predicting difficult laryngoscopy). Moreover, as some of these risk factors, such as age and obesity, are not modifiable (at least in the short term), the actual risk of difficult FMV may be significantly overestimated. Hence, the history of difficult FMV in the patient's medical record becomes a more powerful predictor of future situations; thus, accurate documentation is essential.
Among the available scales for grading technical difficulty in the clinical setting, the one proposed by Han et al. [5] is the most widely used. The Han scale is simple, reproducible, and practical, with each grade conveniently associated with relevant changes in clinical practice. Although subjective, scores will not underestimate the difficulty associated with, for instance, an inexperienced operator or the avoidance of adjuvant maneuvers. The scales proposed by Warters or by Lim-Nielsen have not gained comparable popularity in routine practice because of their complexity and the need for additional monitoring tools.
The easy adoption of the Han scale can partly be explained by its similarity to other “practical” airway-related scales, such as the Cormack-Lehane scale. The latter has undergone several modifications since it was first described. The most widely accepted modification has been the proposed split of Grade 2 into Grades 2a and 2b, which was suggested by Yentis and Lee in 1998. This modification provides additional information regarding the difficulty of intubation, as Grade 2a is associated with potential visualization of the tube passing through the glottis but Grade 2b is not. Various other proposed modifications have not been widely adopted by practitioners, as many are excessively complex and not sufficiently clinically relevant.
Additionally, no consensus regarding the appropriate timing of MR for FMV has been reached. The evidence does not tend to support the clinical practice of systematically checking for adequate FMV prior to MR: the available evidence supports non-checkers more than checkers. Some evidence suggests that loss of muscle tone in the upper airway may lead to airway collapse, which could impair the ventilatory efficiency with FMV under MR in up to a quarter of patients [3]. However, the evidence in favor of “non-checkers” is more robust and recent, with data suggesting improvements in ventilatory capacity both in terms of the ability to facilitate vocal cord opening after induction and improvements in compliance. Additionally, the widespread availability of sugammadex has undoubtedly contributed to the increase in the “non-checker” group, as MR can be reversed rapidly and is thus considerably safer.
The widespread use of laryngeal masks may also have contributed to an increase in the proportion of FMV performed without MR, as the liberal use of relaxants is not warranted. Additionally, as no simple scale is available that provides information on the “relaxation condition” during FMV, it may be under-reported: even if muscle relaxants are not administered prior to FMV, MR is a recognized rescue maneuver recommended by clinical practice guidelines and thus its effect should be adequately recorded in the patient’s history if used [2].
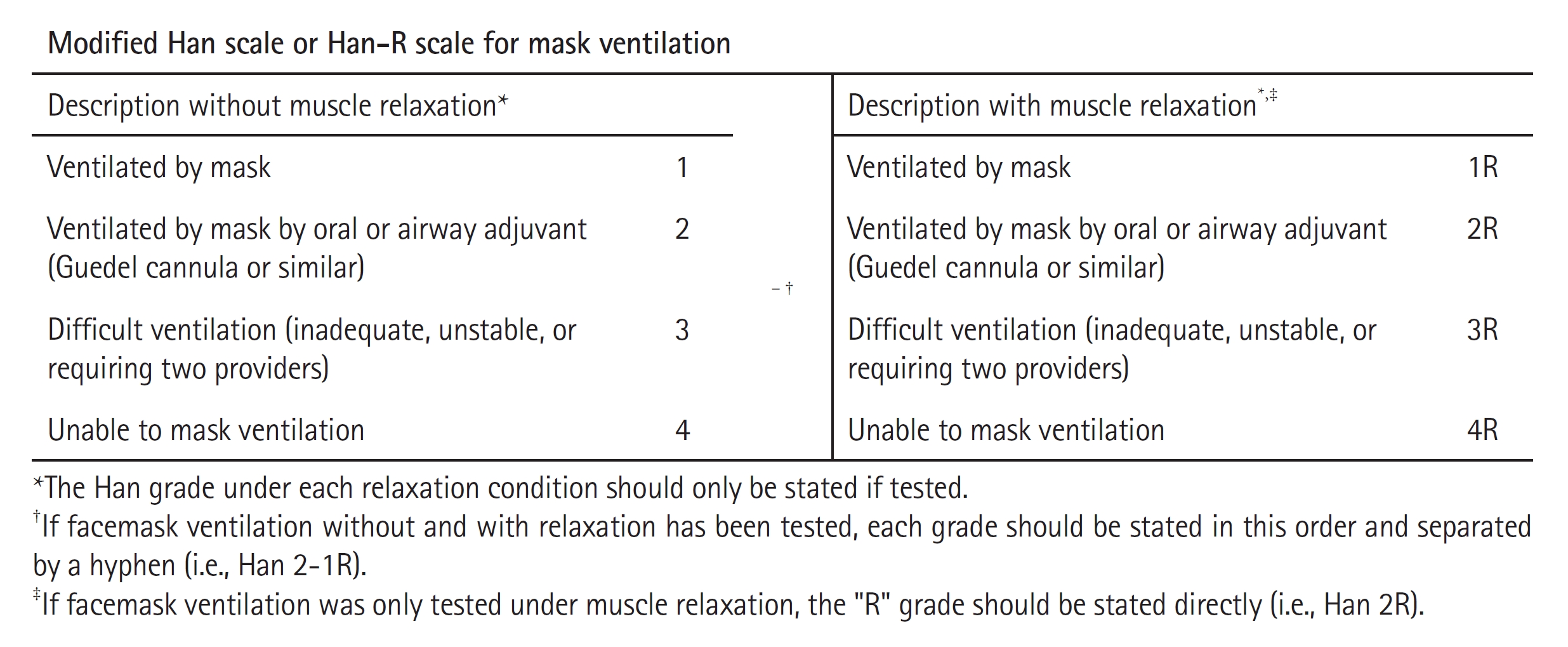
Therefore, we would like to propose the use of a modified Han scale [5] or the “Han-R” scale (Fig. 1). For this proposed scale, the letter “R” is included immediately after the Han grade if ventilation was performed under MR. Consecutive reporting of the Han score in the absence and presence of MR is a simple way to report changes in facilitation of FMV when a state of adequate relaxation is reached. Therefore, a Han 3-2R score would represent a one-grade improvement in FMV difficulty once the muscle relaxant achieves a clinically relevant effect and a Han 2-2R score would represent no change in difficulty after MR. Additionally, a Han 2 score would mean that FMV was conducted without MR, while a Han 2R score would mean that FMV was conducted with MR. The proposed change is a simple way to include valuable information without complicating the format or information provided by the original scale. Splitting the intermediate grades could facilitate early decision-making regarding the use of adjuvants or inclusion of a second operator in subsequent airway approaches, especially in clinical situations with few resources. Furthermore, the proposal does not preclude the use of other scales that would provide information about the quality of the FMV. Finally, no additional effort in routine practice or specific monitoring tools are required for the Han-R scale, making the potential adoption of this scale in day-to-day clinical practice simple and immediate.
In summary, specifying the relaxation status during FMV and any changes in difficulty using the modified Han or “Han-R” scale is a simple way to add important information analogous to specifying the use of BURP or other adjuvant maneuvers alongside the Cormack-Lehane grade in the patient’s medical record.
NOTES
Author Contributions: David Lopez-Lopez (Conceptualization; Investigation; Methodology; Validation; Writing – original draft; Writing – review & editing); Adrian Garcia-Romar (Conceptualization; Visualization; Writing – review & editing); Patricia Neira Somoza (Conceptualization; Methodology; Writing – review & editing); Pablo Casas-Reza (Supervision; Writing – review & editing); Rocio Mato-Bua (Conceptualization; Supervision)
References
1. Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015; 115: 827-48.



2. Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology 2022; 136: 31-81.



3. Ramachandran SK, Kheterpal S. Difficult mask ventilation: does it matter? Anaesthesia 2011; 66 Suppl 2: 40-4.