 |
 |
| Korean J Anesthesiol > Volume 77(2); 2024 > Article |
|
Abstract
Background
Methods
Results
NOTES
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (Ministry of Science and ICT) (Grant number: RS-2022-00165755). This study was also supported by grants (2023IE0008 and 2023IP0134) from the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Republic of Korea.
Data Availability
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Author Contributions
Ji-Hoon Sim (Data curation; Formal analysis; Funding acquisition; Methodology; Resources; Validation; Writing – original draft)
Chan-Sik Kim (Conceptualization; Data curation; Formal analysis; Methodology; Writing – original draft)
Seungil Ha (Data curation; Formal analysis; Investigation; Methodology; Project administration)
Hyunkook Kim (Formal analysis; Investigation; Methodology; Resources; Validation)
Yong-Seok Park (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Writing – review & editing)
Joung Uk Kim (Data curation; Supervision; Validation; Visualization)
Fig. 1.
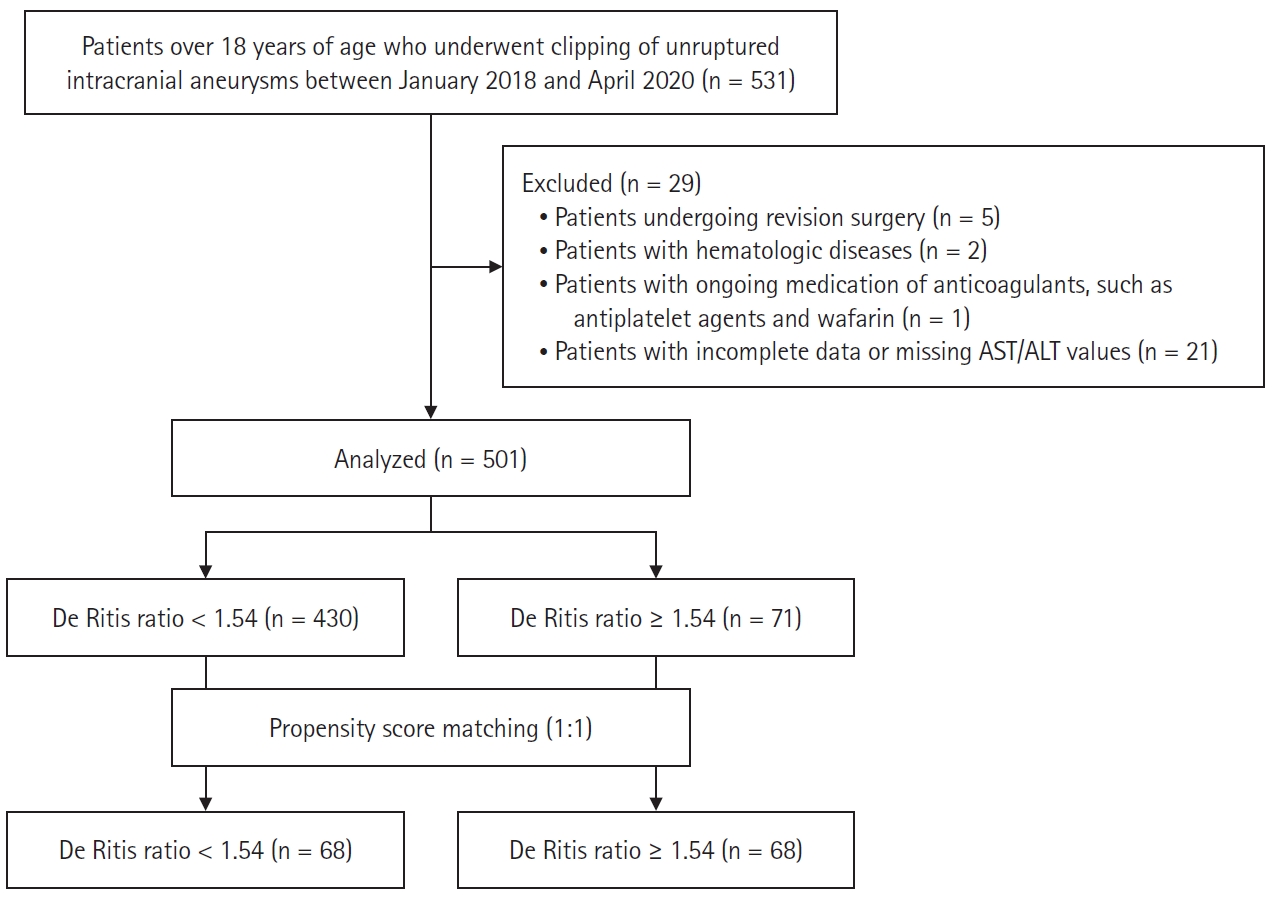
Fig. 2.

Table 1.
Values are presented as mean ± SD, median (Q1, Q3), or number (%). SMD: standardized mean difference, DM: diabetes mellitus, HTN: hypertension, CVD: cardiovascular disease, CVA: cerebral vascular accident, CKD: chronic kidney disease, ACA: anterior cerebral artery, MCA: middle cerebral artery, ICA: internal carotid artery, WBC: white blood cell, PT: prothrombin time, INR: international normalized ratio, aPTT: activated partial thromboplastin time, BUN: blood urea nitrogen, RDW: red blood cell distribution width, CRP: C-reactive protein, BMI: body mass index, AST: aspartate aminotransferase, ALT: alanine aminotransferase, RBC: red blood cell.
Table 2.
Table 3.
Values are presented as median (Q1, Q3). AUC: area under the curve, NRI: net reclassification improvement, IDI: integrated discrimination improvement, BMI: body mass index, CVD: cardiovascular disease, PT: prothrombin time, INR: international normalized ratio, Hb: hemoglobin. *Model 1 = age + BMI + sex + CVD + Hb + PT, INR + albumin.









