 |
 |
| Korean J Anesthesiol > Volume 77(1); 2024 > Article |
|
Median sternotomy is the standard approach for cardiac surgery (CS). However, conventional CS has some disadvantages such as severe pain, a long hospital stay, and cosmetic concerns. Minimally invasive cardiac surgery (MICS) is not associated with these disadvantages [1]. MICS facilitates earlier mobilization and faster postoperative recovery. Incision types for MICS include upper/lower hemisternotomy and right/left anterior minithoracotomy. An incision is made at the level of the second, third, or fourth intercostal space, with the patient in the supine position [1]. Patients may experience severe pain due to the involvement of the intercostal nerves and rib retraction [1]. The serratus anterior plane block (SAPB), erector spinae plane block (ESPB), transverse thoracic muscle plane block (TTMPB), and pecto-intercostal fascial plane block (PIFPB) may be used for analgesia after MICS [2–4]. The serratus posterior superior intercostal plane block (SPSIPB) is a novel block that is performed between the serratus posterior superior (SPSm) and the intercostal (ICm) muscles [5]. As an example for thoracic analgesia, the SPSIPB has been used to provide analgesia after breast surgery [5]. Our aim here is to report on our experience with administering SPSIPBs for left-sided MICS in three patients. Written informed consent was obtained from all the patients.
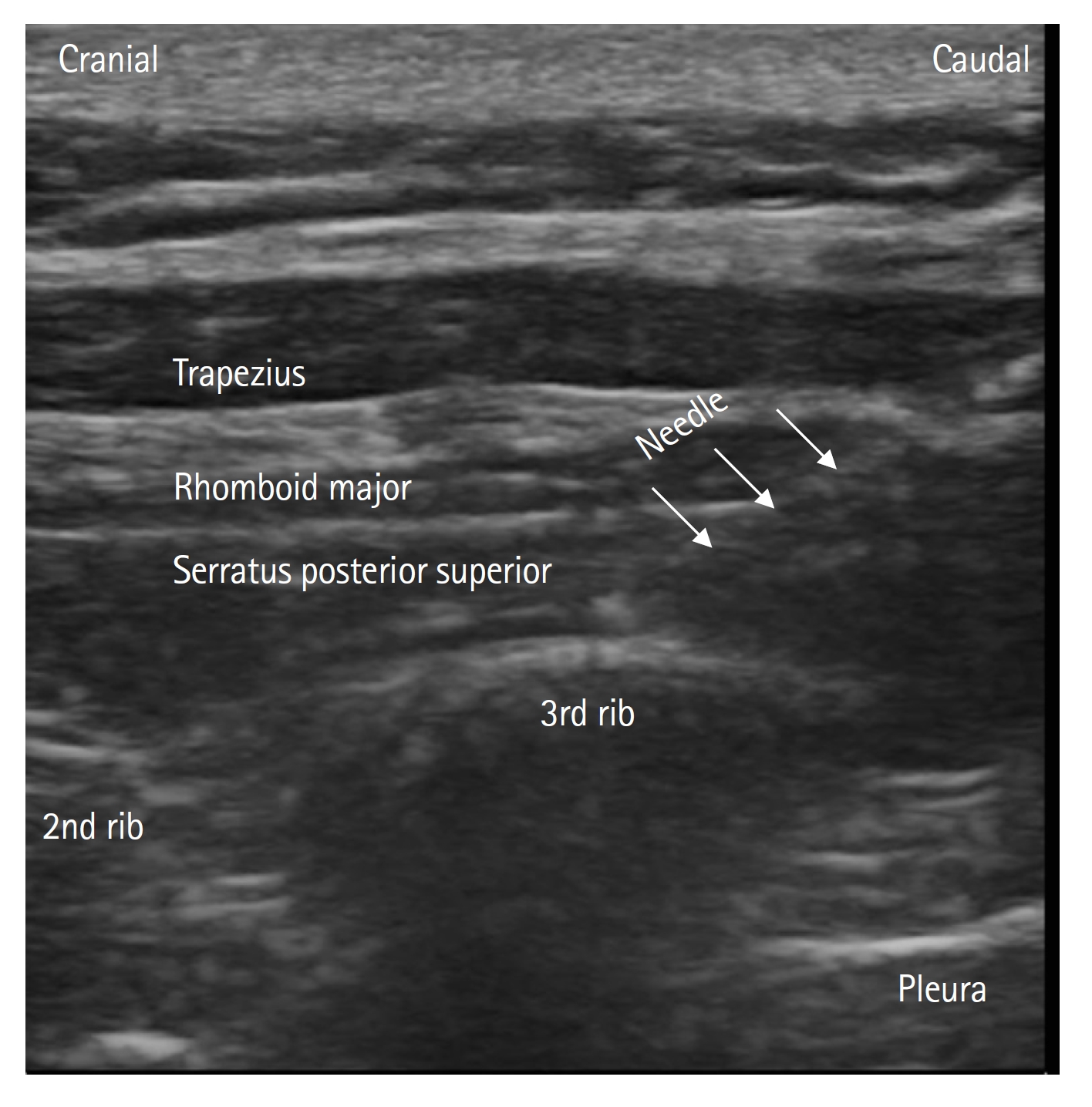
The demographics of the patients were as follows: male aged 50 years (Patient 1), female aged 53 years (Patient 2), and female aged 47 years (Patient 3). The height/weight of the patients were 172 cm/75 kg, 168 cm/80 kg, and 160 cm/70 kg, respectively. At the end of surgery, each patient underwent an SPSIPB in the lateral decubitus position. A linear probe was placed near the medial border of the scapula and a 22-G, 80-mm block needle (Stimuplex® Ultra 360®, B-Braun) was inserted between the third rib and the SPSm (Fig. 1). After correction, 30 ml of 0.25% bupivacaine was administered. Ibuprofen 400 mg and tramadol 100 mg were administered intravenously at the end of surgery. All patients were transferred to the cardiovascular intensive care unit (CVICU) after surgery and were attached to a patient-controlled analgesia (PCA) device containing tramadol (2 mg/ml, 10-mg bolus, 7 mg/h infusion, 20-min lockout, and 4 h). Patients were extubated 2 h after admission to the CVICU. 400 mg of ibuprofen was administered intravenously every 8 h. Pain was evaluated using the numerical rating scale (NRS) and the sedation level was assessed using a 4-point sedation scale during the NRS evaluation. The sedation level of all the patients was zero during assessments. The NRS scores at 2, 4, 8, 16, and 24 h were 1/1/3/2/0 for Patient 1, 1/1/2/1/0 for Patient 2, and 1/2/3/2/1 for Patients 3, respectively. The blockade lasted a maximum of 8 h. The posteroanterolateral dermatomal coverage (pin-prick test) was between C5-T8, C5-T7, and C6-T8 for each patient, respectively. The PCA dose administered to each patient was a 20-mg bolus.
The use of SAPBs in cardiothoracic surgery is a safe and effective option for postoperative pain [2]. The SAPB targets the lateral branches of the intercostal nerves. As these nerves receive sensory innervation from the anterolateral thorax, the SAPB only provides anterolateral hemithoracic analgesia. In contrast, the SPSIPB provides anteroposterior thoracic analgesia, as a recent report shows dye spreading from the C7 to the T7 ICm and nerves [5]. Based on the spread pattern, the SPSIPB may be a better choice than the SAPB for CS. However, the patient must be moved to the lateral decubitus position for the SPSIPB, while the SAPB can be performed after MICS without any positional changes. This can be a significant limitation for the use of SPSIPB in MICS. This position makes the paravertebral block (PVB) easier to perform than the SPSIPB. The PVB, however, is associated with a high risk of complications such as pneumothorax and vascular injury; thus the SPSIPB is safer than the PVB. The ESPB is effective for analgesia after CS. However, it was recently reported that ESPB was not associated with a significant reduction in pain after CS [3]. The TTMPB, which is performed between the transverse thoracic muscle and the ICm, provides effective analgesia management following CS; however, the area of block coverage is close to the blood vessels and pleura [4]. The PIFPB is performed between the pectoralis major muscle and the ICm [4]. However, the PIFPB fails to cover the T6 level. Both the TTMPB and PIFPB are close to the surgical area, and their effectiveness may be affected by the type of surgery.
In conclusion, we evaluated the efficacy of SPSIPB in patients who underwent MICS. SPSIPB provides effective analgesia management after MICS. A randomized controlled trial would be better suited to accurately judge the feasibility of the SPSIPB, rather than a case report.
NOTES
Author Contributions: Bora Bilal (Conceptualization; Investigation; Methodology; Writing – original draft; Writing – review & editing); Bahadir Ciftci (Conceptualization; Investigation; Methodology; Writing – original draft; Writing – review & editing); Selcuk Alver (Conceptualization; Investigation; Methodology; Writing – original draft; Writing – review & editing); Ali Ahiskalioglu (Conceptualization; Investigation; Methodology; Writing – original draft; Writing – review & editing); Serkan Tulgar (Conceptualization; Investigation; Methodology; Writing – original draft; Writing – review & editing)
Fig. 1.
Sonoanatomy and needle direction during serratus posterior superior intercostal plane block. The trapezius, rhomboid major, and serratus posterior superior muscles; second and third ribs; and the pleura are visible as anatomical landmarks. The needle is facing the cranio-caudal direction. The needle tip is visible just over the third rib.
References
1. Onan B. Minimal access in cardiac surgery. Turk Gogus Kalp Damar Cerrahisi Derg 2020; 28: 708-24.



2. Patel SJ, Augoustides JG. Serratus anterior plane block-a promising technique for regional anesthesia in minimally invasive cardiac surgery. J Cardiothorac Vasc Anesth 2020; 34: 2983-5.


3. King M, Stambulic T, Servito M, Mizubuti GB, Payne D, El-Diasty M. Erector spinae plane block as perioperative analgesia for midline sternotomy in cardiac surgery: a systematic review and meta-analysis. J Card Surg 2022; 37: 5220-9.



4. Kaya C, Dost B, Dokmeci O, Yucel SM, Karakaya D. Comparison of ultrasound-guided pecto-intercostal fascial block and transversus thoracic muscle plane block for acute poststernotomy pain management after cardiac surgery: a prospective, randomized, double-blind pilot study. J Cardiothorac Vasc Anesth 2022; 36: 2313-21.


-
METRICS

-
- 1 Crossref
- Scopus
- 1,370 View
- 146 Download








