Corrosive poisoning and its implications on pediatric airways
Article information
Pharyngeal webs are a rare anomaly that occur after corrosive ingestion due to liquefaction necrosis (bases) or coagulation necrosis (acids). The mucosal lining heals by fibrosis, causing upper airway stenosis, synechiae, band formation, and esophageal stricture. In India, corrosive poisoning poses a large burden on the healthcare system, accounting for approximately 2% of the total cases of poisoning, and is associated with high morbidity and mortality, estimated at 50% and 13%, respectively [1].
For these patients, securing the airway is an anesthetic challenge owing to the distorted anatomy of the upper airway. Drooling and an inability to swallow indicate severe posterior pharyngeal or upper esophageal injury. The presence of hoarseness, stridor, nasal flaring, or rib retraction upon inhalation suggest airway involvement [2]. Multiple endoscopic or open procedures may be required to treat complications like pharyngeal and laryngeal webs, synichae and esophageal stricture. Airway management is thus both complicated and of paramount importance. Here, we discuss the challenges faced and measures taken to secure the airway in a pediatric patient with post-corrosive esophageal stricture posted for feeding jejunostomy.
A 14-year-old female with a history of corrosive poisoning in May 2022 presented with an esophageal stricture and was posted for feeding jejunostomy. She had previously undergone upper gastrointestinal endoscopy and esophageal dilatation six times. Preoperative airway examination revealed mouth opening of three fingers, a Mallampati score of II (Fig. 1A), stable vitals, and all routine investigations within normal limits. Written informed consent was obtained from the parents. Anticipating a difficult airway, the patient was attached to operation theatre standard monitors, with a fiberoptic flexible bronchoscope video scope (Storz®, Karl Storz Endoskope, Karl Storz Endoscopy India pvt Ltd., India) at the ready, and the cricothyroid membrane was marked using the laryngeal handshake technique. Pre-oxygenation was initiated with 100% oxygen using a closed circuit and intravenous (IV) fentanyl 2 μg/kg and propofol 2 mg/kg were administered for induction. A size 2.5 i-gel® supraglottic airway device (Intersurgical complete respiratory system, UK) was introduced, which had a significant leak. A size 3 i-gel® supraglottic airway device (Intersurgical complete respiratory system, UK) was then introduced, which also had a leak. As mask ventilation was possible, tracheal intubation using succinylcholine 1.5 mg/kg was conducted. Direct laryngoscopy revealed a distorted airway, with multiple visible webs and openings. The epiglottic tip was identified with great difficulty as it was embedded in the scar tissue. Because we were unsure of the location of the trachea, a fiberoptic bronchoscope was used for identification (Fig. 1B). The trachea was confirmed by direct visualization of the tracheal rings and carina, and the endotracheal tube was railroaded over the flexible bronchoscope (Fig. 1C). The position of the tube was confirmed by bronchoscopy and end-tidal CO2. IV dexamethasone (8 mg), hydrocortisone (100 mg), and vecuronium (0.1 mg/kg) were administered after the effect of succinylcholine subsided. Anesthesia was maintained with 50% oxygen and 2 L total flow with sevoflurane at 1 minimum alveolar concentration. Once the surgical procedure was completed, the ENT team was called for endoscopy and ablation of the synechiae. The neuromuscular blocking agents were reversed with 100% oxygen, IV neostigmine (0.04 mg/kg body weight), and IV glycopyrrolate (0.01 mg/kg body weight). Once fully awake, the patient was extubated and transferred to the post-anesthesia care unit for observation.
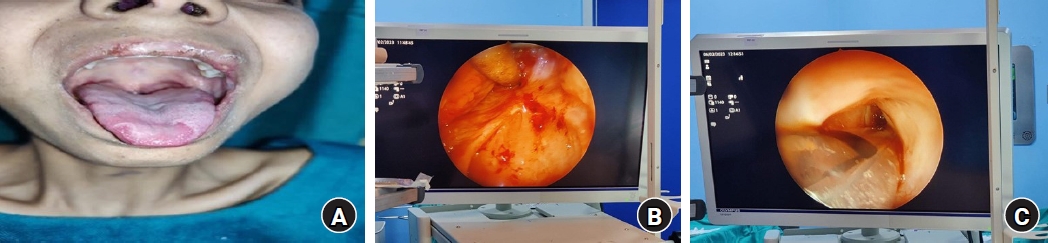
(A) Modified Mallampati score of II. (B) Pharyngeal web seen on fiberoptic bronchoscopy. (C) Endotracheal tube passing through the vocal cords.
Although the airway examination was normal in the preoperative evaluation, a difficult airway should be anticipated in patients with a history of corrosive poisoning and appropriate arrangements should be made. The use of a laryngeal mask airway is limited to patients with normal upper airway anatomy and is thus seldom used in those with distorted airway conditions. The hallmark of management in these cases includes preservation of spontaneous ventilation until confidence in the airway is reached following laryngoscopy. Intubation must be performed under visual guidance to avoid passage into a false track or incorrect placement of endotracheal tube [3].
Airway mismanagement remains an important cause of mortality and morbidity in anesthetic practice. Conventional rigid direct laryngoscopy aids tracheal intubation in 98.1% of the cases [4]. Thus, alternative equipment and techniques must be readily available for the remaining 1.9% of cases. These patients can also have tracheal stenosis; thus, a preoperative neck radiograph (AP, lateral view) or computed tomography is advised, and smaller endotracheal tubes and a backup for front-of-neck access should be arranged.
We conclude that every case of post-corrosive poisoning, acute or chronic, that requires tracheal intubation should be defined as a difficult airway case and appropriate arrangements according to available guidelines must be made to prevent airway mishaps [5].
Notes
Funding: None.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
Author Contributions: Yashwant Singh Payal (Conceptualization; Supervision); Sachin Sogal P (Formal analysis; Project administration); Pooja CS (Data curation; Resources; Writing – original draft)
