 |
 |
| Korean J Anesthesiol > Volume 76(5); 2023 > Article |
|
Abstract
Background
Methods
Results
NOTES
Data Availability
Availability of data: template data collection forms, data extracted from included studies, data used for all analyses on other data are available from the corresponding author on request.
Author Contributions
Valery V. Likhvantsev (Conceptualization; Writing – original draft; Writing – review & editing)
Giovanni Landoni (Conceptualization; Writing – original draft; Writing – review & editing)
Levan B. Berikashvili (Formal analysis; Writing – original draft)
Nadezhda V. Ermokhina (Formal analysis)
Mikhail Y. Yadgarov (Formal analysis; Writing – original draft)
Yuki Kotani (Formal analysis; Writing – original draft)
Kristina K. Kadantseva (Formal analysis)
Dmitry M. Makarevich (Formal analysis; Writing – original draft)
Andrey V. Grechko (Formal analysis; Writing – original draft)
Supplementary Materials
Supplementary Material 1.
Supplementary Table 1.
Supplementary Table 2.
Supplementary Fig. 1.
Supplementary Fig. 2.
Supplementary Fig. 3.
Supplementary Fig. 4.
Supplementary Fig. 9.
Fig. 1.

Fig. 2.

Fig. 3.
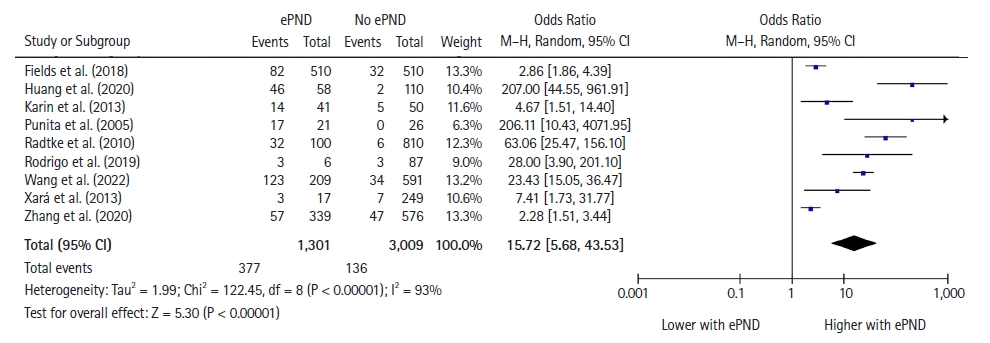
Table 1.
| Study | Design | ePND criteria | Scale type | Sample size, ePND (%) | Mean age (yr) | Sex, male (%) | ASA≥ 3, (%) | Volatile anesthetics (% of patients) | Operation time (min) | Anesthesia time (min) |
|---|---|---|---|---|---|---|---|---|---|---|
| Assefa and Sahile (2019) [22] | PO | RASS ≥ +1 | Motor | 306, 97 (32%) | 44 | 47 | 2.6 | N/D | 65.5 | N/D |
| Fields et al. (2018) [23]* | Matched case-control | RASS score of +3 or +4 or the administration of haloperidol | Motor | 1020, 510 (50%) | 63 | 73 | N/D | 44 | 138 | N/D |
| Gutiérrez et al. (2019) [24] | PO | CAM | Cognitive | 93, 6 (6%) | 73 | 39 | N/D | N/D | N/D | N/D |
| Hesse et al. (2019) [25] | PO | CAM-ICU | Cognitive | 626, 125 (20%) | 59 | 60 | 43 | 98 | N/D | 116 |
| Huang et al. (2020) [26] | PO | Nu-DESC | Cognitive | 168, 58 (35%) | 72 | 53 | 55 | 100 | 141 | N/D |
| Kim et al. (2015) [27] | RO | SAS ≥ 5 | Motor | 488, 48 (10%) | 62 | 82 | 6.2 | 92 | 109 | 146 |
| Lepouse et al. (2006) [28] | PO | SAS ≥ 5 | Motor | 1359, 64 (5%) | 51 | 54 | 21 | 64 | 76 | N/D |
| Munk et al. (2016) [29] | PO | RASS ≥ +1 | Motor | 1970, 73 (4%) | 60 | 46 | 15 | 11 | 80 | 147 |
| Neufeld et al. (2013) [30] | PO | DSM-IV | Cognitive | 91, 41 (45%) | 79 | 42 | N/D | N/D | 186 | N/D |
| Olbert et al. (2019) [31] | PO | DSM-V | Cognitive | 176, 16 (9%) | 69 | 54 | 30 | N/D | N/D | 130 |
| Sharma et al. (2005) [32] | PO | CAM | Cognitive | 47, 21 (45%) | 77 | 34 | 2 | 100 | 145 | N/D |
| Radtke et al. (2008) [33] | PO | DSM-IV | Cognitive | 154, 21 (14%) | 54 | 60 | 25 | 55 | 75 | N/D |
| Radtke et al. (2010) [34] | PO | Nu-DESC | Cognitive | 910, 100 (11%) | 53 | 53 | 26 | 53 | 79 | N/D |
| Radtke et al. (2010) [35] | PO | RASS ≥ +1 | Motor | 1868, 93 (5%) | 52 | 51 | 29 | 61 | 84 | N/D |
| Saller et al. (2019) [36] | PO | DSM-V | Cognitive | 543, 22 (4%) | 52 | 55 | 21 | 41 | 97 | N/D |
| Wang et al. (2020) [37] | PO | CAM-ICU | Cognitive | 800, 209 (26%) | 48 | 41 | 3.5 | N/D | 261 | N/D |
| Wiinholdt et al. (2019) [38] | PO | Nu-DESC | Cognitive | 1000, 103 (10%) | 60 | 48 | 20 | 72 | N/D | 141 |
| Winter et al. (2015) [39] | PO | Nu-DESC ˃ 2 | Cognitive | 1000, 43 (4%) | 58 | 40 | 9.3 | N/D | 93 | 166 |
| Wu et al. (2021) [40] | PO | CAM-ICU | Cognitive | 228, 57 (25%) | 39 | 43 | 13 | 82 | N/D | N/D |
| Xará et al. (2013) [41] | PO | RASS ≥ +1 | Motor | 266, 17 (6%) | 56 | 40 | 16 | N/D | 90 | N/D |
| Yu et al. (2010) [42] | PO | Three point scale | Motor | 2000, 426 (21%) | 42 | 43 | 0 | 68 | N/D | N/D |
| Zhang et al. (2020) [43] | PO | СAM-ICU | Cognitive | 915, 339 (37%) | 71 | 60 | 0 | 31 | 203 | N/D |
*This case-control study was excluded from the occurrence rate of ePND and mortality rate calculations of the included studies overall. ePND: early postoperative neurocognitive disorders, SAS: Riker Sedation–Agitation Scale, ASA: American Society of Anesthesiologists, RASS: Richmond Agitation-Sedation Scale, CAM: Confusion Assessment Method, CAM-ICU: Confusion Assessment Method for the Intensive Care Unit, Nu-DESC: Nursing-Delirium Screening Scale, DSM: Diagnostic and Statistical Manual of Mental Disorders, RO: retrospective observational, PO: prospective observational, N/D: no data.
Table 2.
Table 3.
ePND: early postoperative neurocognitive disorder, ED: emergence delirium, EA: emergence agitation, POD: postoperative delirium, OR: odds ratio, SMD: standardized mean difference, PACU: post anesthesia care unit, LoS: length of stay. Key; 0: no evidence downgrade, −1: serious limitation, −2: very serious limitation, +1: evidence upgrade. Baseline evidence level for studies of prognostic factors: high. *Therapy for early postoperative neurocognitive disorders in the ePND group could potentially decrease POD rates.
References
- TOOLS
-
METRICS

-
- 0 Crossref
- 1 Scopus
- 2,211 View
- 122 Download








