Comparison of the pericapsular nerve group block with the intra-articular and quadratus lumborum blocks in primary total hip arthroplasty: a randomized controlled trial
Article information
Abstract
Background
The pericapsular nerve group (PENG) block, quadratus lumborum block (QLB), and intra-articular (IA) local anesthetic injection have been shown to provide effective analgesia in total hip arthroplasty (THA). This randomized study aimed to compare the analgesic efficacy, motor protection, and quality of recovery associated with the PENG block, QLB, and IA injection.
Methods
Eighty-nine patients who underwent a unilateral primary THA under spinal anesthesia were randomly assigned to the PENG (n = 30), QLB (n = 30), or IA (n = 29) group. The primary outcome was the numerical rating scale (NRS) score over the first 48 h postoperatively. The secondary outcomes were postoperative opioid consumption, quadriceps and adductor muscle strength, and quality of recovery (QoR-40).
Results
The dynamic (with movement) NRS scores at 3 and 6 h postoperatively were significantly lower in the PENG and QLB groups compared to the IA group (P = 0.002 and P < 0.001, respectively). The time to first opioid analgesia requirement was longer in the PENG and QLB groups than in the IA group (P = 0.009 and P = 0.016, respectively). A provided better preservation was found in the the PENG group than in the QLB group in terms of quadriceps muscle strength at 3 h postoperatively (P = 0.007) and time to mobilization (P = 0.003). No significant differences in the QoR-40 scores were seen.
Conclusions
The PENG and QLB groups showed similar analgesic effects and both showed more effective analgesia 6 h postoperatively than the IA group. All the groups showed similar postoperative quality of recovery.
Introduction
As the hip joint receives sensory innervation from both the lumbar and sacral plexuses, providing effective regional analgesia to this area is difficult [1]. Additionally, the method used for postoperative analgesia after hip surgery must both provide effective analgesia and allow for mobilization as early as possible [1,2]. Ideally, this process should also have a motor protective effect to reduce the risk of thromboembolic events and increase functional improvement by shortening the length of hospital stay [3].
The pericapsular nerve group (PENG) block described in 2018 by Giron-Arango et al. [4] can be used for hip surgery. In hip fracture surgery and elective arthroplasty, a preoperative and postoperative analgesic blockade is applied to the obturator, femoral, and accessory obturator nerves, which innervate the anterior side of the hip joint [5]. With the PENG block, only the sensory branches of the femoral nerve that travel to the hip joint are blocked; no motor blockade occurs [6]. Consequently, excellent analgesia can be provided without affecting muscle strength, which facilitates postoperative functional recovery.
The quadratus lumborum block (QLB), first described by Blanco [7] in 2007, is administered around the quadratus lumborum muscle (QLM). The QLM is located between the middle and anterior thoracolumbar fascia adjacent to the fascia of the psoas major muscle (PM) medially and the transversalis fascia laterally. The name changes according to the point of injection [8–10]. In earlier studies, the anterior QLB was also classified as the transmuscular approach (between the QLM and PM) [11]. Owing to its anatomical proximity to the QLM, the QLB is thought to have a large blocking capacity through affecting the L1-3 nerve root. Cadaveric studies have shown that the anterior and subcostal QLB cover nerves that provide sensory innervation to the hip [8,9]. The QLB has also been shown to provide effective analgesia for total hip arthroplasty (THA) without causing weakness in the quadriceps muscles [10].
Intra-articular (IA) local anesthetic injections, which are practical and easy to administer, have been reported to result in lower postoperative pain scores and opioid compared to non-administered group in previous studies on hip arthroplasty [12,13].
We hypothesized that patients undergoing THA who received the PENG block would have lower numerical rating scale (NRS) scores and opioid consumption and better motor protection and quality of recovery (QoR) than those who received the QLB and IA injection. The primary outcome of this prospective randomized study was the severity of pain represented by the NRS score of patients undergoing THA, measured in the first 48 h after receiving the PENG block, QLB, and IA injection. The secondary outcomes included postoperative opioid consumption, time to first mobilization, quadriceps muscle strength, hip adduction strength, and QoR (according to the QoR-40).
Materials and Methods
The study protocol was approved by the Ethics Committee of Karamanoğlu Mehmetbey University Faculty of Medicine (decision no: 04-2021/14, June 23, 2021). This trial was registered at ClinicalTrials.gov (NCT05003544). Written informed consent was obtained from all patients who participated in the study, in accordance with the principles of the Declaration of Helsinki, 2013.
Patients aged 18–85 years who underwent unilateral primary THA with spinal anesthesia administered in accordance with the American Society of Anesthesiologists (ASA) I–III criteria between August 12, 2021 and January 31, 2023 were included in the study. The exclusion criteria were as follows: a history of surgery on the same hip, liver or kidney failure, allergy or intolerance to one of the study drugs, body mass index > 40 kg/m2, ASA phsyical status score of IV, or long-term use of gabapentin/pregabalin or opioids.
Patient randomization was performed at a ratio of 1 : 1 : 1 basis by an expert who was not involved in the study using a computer-generated program (https://www.randomizer.org). Patients were assigned to one of three groups (30 patients each) using computer-generated random numbers and coded sealed opaque envelopes that were opened immediately before performing the PENG block (PENG group), QLB (QLB group), or IA injection (IA group). A specialist who did not perform the preoperative block and was blinded to the patient groups performed the postoperative evaluation. The postoperative pain assessment specialists, nurses, and patients were all blinded to the intervention group, including during the data collection process.
As part of the multimodal analgesia, 1,000 mg paracetamol was administered intravenously (IV) in the preoperative holding area. Patients were followed up in a standard manner. Subsequently, 2 mg IV midazolam, 40 mg IV esomeprazole, and 4 mg IV dexamethasone were administered. After the patients were positioned appropriately for spinal anesthesia, 2.2 ml of 0.5% hyperbaric bupivacaine was injected into the L3-4 intervertebral space. The posterolateral surgical approach was used in all patients in the lateral decubitus position.
For postoperative analgesia, patients were routinely administered 1,000 mg IV paracetamol three times a day and 50 mg oral diclofenac every 8 h (25 mg if aged ≥ 75 years). In addition, 5 mg oral oxycodone was administered to patients with an NRS score > 4.
Sham procedure
The sham block procedure was applied to all patient groups. When applying the sham procedure, the QLB and PENG block protocols were performed using a simulation method. The simulation QLB was applied to the PENG group, the PENG simulation to the QLB group, and both block simulation the IA group. The practitioner simulated these blocks after the QLB and PENG block positions were assigned to all participating patients. After probe placement in a QLB- and PENG block-like manner, a sufficient pause was allowed to simulate a blunt needle, then a 20 ml syringe with saline, without administering any medication.
PENG block technique
For the PENG block, sterile conditions were maintained with the patient in the supine position. A low-frequency convex ultrasound transducer (Samsung RS85 Prestige®, Republic of Korea) was placed in the anteroinferior iliac spine. The probe was placed a transverse orientation, medical, and caudal to the anterosuperior iliac spine in order to identify the anteroinferior iliac spine, the iliopubic eminence, and the psoas tendon. After the psoas tendon was visualized, with a 21-gauge 100-mm block needle (B. Braun®, Germany), the tip of the psoas tendon was determined using the in-plane technique with a lateral-to-medial approach (Fig. 1A). Following negative aspiration, 20 ml of 0.5% bupivacaine was injected under the psoas tendon and local anesthetic spread was observed (Fig. 1B).
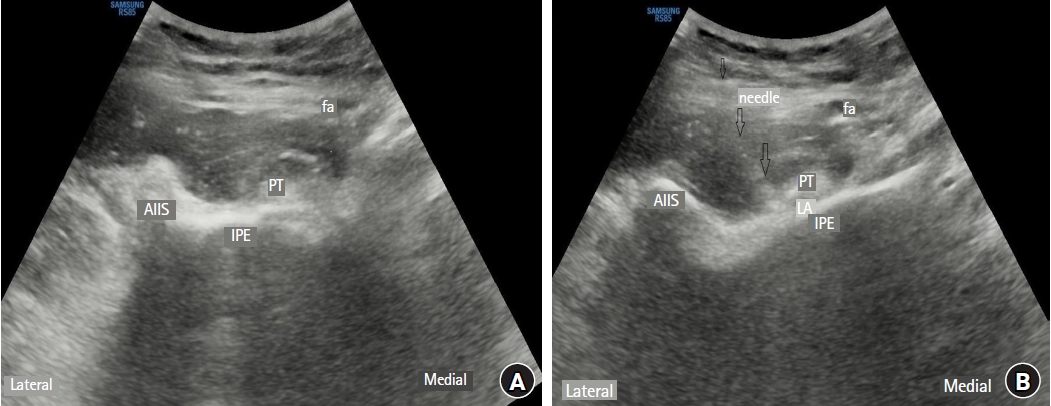
Pericapsular nerve group block. (A) A low-frequency curvilinear was placed in a transverse orientation, medial and caudal to the anterosuperior iliac spine in order to identify the anterior inferior iliac spine, the iliopubic eminence, and the psoas muscle tendon. (B) The needle placement between the psoas muscle tendon and the iliopubic eminence with a lateral-to-medial approach using the in-plane technique. After negative aspiration, local anesthetic spread was observed under the psoas muscle tendon. AIIS: anterior inferior iliac spine, fa: femoral artery, IPE: iliopubic eminence, PT: psoas muscle tendon, LA: local anesthesia.
QLB technique
For the anterior QLB, the patients were positioned laterally with the surgical side facing up. A low-frequency convex ultrasound probe was placed at the level of the L4 spine with the iliac wing. When the “Shamrock” appearance (Fig. 2A) was visualized, a 21-gauge 100-mm block needle was advanced to the QLM in the posterior to anterior direction using the in-plane technique and the needle tip was inserted between the PM and the fascial space of the QLM. Following negative aspiration, 30 ml of 0.5% bupivacaine was slowly injected into the fascial area (Fig. 2B). Block success was confirmed by observing the separation of the QLM and PM in the same plane.
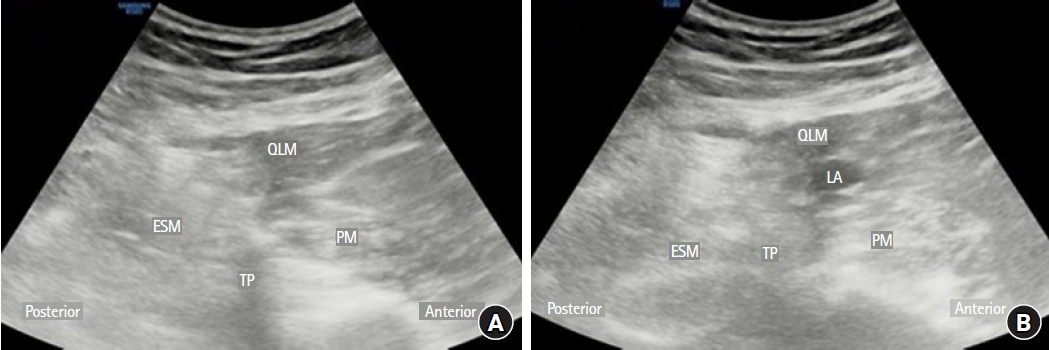
Anterior quadratus lumborum block. (A) A low-frequency convex ultrasound probe was placed at the level of the L4 spine with the iliac wing. Subsequently, the L4 vertebral body at the L4 vertebra level, along with the L4 transverse process, the quadratus lumborum, the erector spinae muscle, and the psoas muscle, were identified as the Shamrock sign. (B) The needle placement between the QLM and the psoas muscle with a posterior-to-anterior approach using the in-plane technique. After negative aspiration, local anesthetic spread was observed between the QLM and the psoas muscle. QLM: quadratus lumborum muscle, ESM: erector spinal muscle, PM: psoas muscle, TP: transverse process, LA: local anesthesia.
IA injection
After the placement of the hip prosthesis, 30 ml of 0.5% bupivacaine and 30 ml of saline were administered by IA injection after the joint capsule was closed.
Outcome measurements
The primary outcome measure was the maximum severity of pain perceived at all postoperative time points (3, 6, 8, 12, 24, and 48 h) using an NRS pain score ranging from 0–10. The NRS value was evaluated as rest (static) and during movement (dynamic) for the first 48 h postoperatively.
The secondary outcomes were the time to first postoperative opioid requirement and opioid consumption (reported in oral morphine equivalents within the first 48 h postoperatively). Quadriceps motor function was evaluated at 3, 6, 12, and 24 h postoperatively with the hip and knee flexion test at 45º and 90º, respectively (normal strength = 0 points [extension against resistance]; paresis = 1 point [flexion against gravity but not against resistance]; and paralysis = 2 points [no extension]). An inflated blood pressure cuff was placed at 40 mmHg of hip adduction force and the patient was instructed to compress the cuff as hard as possible and maintain this effort. The percent reduction in strength compared with the baseline measurement was scored as follows: 0%–20% = 0 points, 21%–70% = 1 point, and 71%–90% = 2 points [14,15]. QoR was evaluated on postoperative days 1, 2, and 7 using the QoR-40 questionnaire. The development of nausea, vomiting, pruritus, urinary retention, or respiratory depression was recorded, and patient satisfaction was evaluated.
Statistical analysis
The sample size was calculated for the one-way analysis of variance (ANOVA), which was used to test the main hypothesis of the study (comparison of NRS scores between the three independent groups). Before starting the study, a power analysis was performed with reference to the literature [16] and expert opinion. The effect size was calculated using the mean postoperative (0–12 h) NRS values obtained from the literature (the mean NRS values of the PENG and control groups were 2.5 and 5.5, respectively; the mean NRS value of the QLB was estimated to be 4 based on expert opinion; and standard deviations were homogeneous and the mean was 3) [16,17]. Cohen’s effect size was calculated as 0.408 using the group mean and standard deviation values. To reach a minimum power of 90% (1-β = 0.10) with α = 0.05 error (95% confidence interval, CI) for the ANOVA test, the minimum number of patients to include in the study was determined to be 81 (27 patients in each group). Considering a potential loss to follow-up for any reason of 10%, 90 patients (30 patients in each group) were included in the study. G*Power (version 3.1.9.5; Heinrich-Heine-Universität, Germany) was used for sample size estimation.
Statistical data analyses were conducted using IBM® SPSS® Statistics software (version 22; IBM Corp., USA). Descriptive categorical data are presented as numbers (n) and percentages (%). The chi-square or Fisher’s exact test was used, depending on the sample sizes in the crosstab cells, to compare the ratios between categorical variables. Descriptive statistics of numerical data are presented as mean ± standard deviation or median (Q1, Q3) values, depending on whether the data were normally distributed. The Shapiro-Wilk test and some graphical methods (histogram and Q-Q plots) were used to determine the conformity of the data to a normal distribution. One-way ANOVA was used to compare normally distributed numerical data among the three independent groups, and the Kruskal-Wallis test was used to compare non-normally distributed data.
For comparisons showing significant differences in the ANOVA, the Tukey test was conducted, and the Kruskal-Wallis test was followed by Dunn-Bonferroni post-hoc pairwise comparison tests. A two-way mixed ANOVA was used as parametric test. The effect of the research groups on the change in the repeated measurements of NRS values at rest (static) and during movement (dynamic) measured at seven different time points (Supplementary Material 1). All statistical tests were two-sided, and the level of statistical significance was set at P < 0.05.
Results
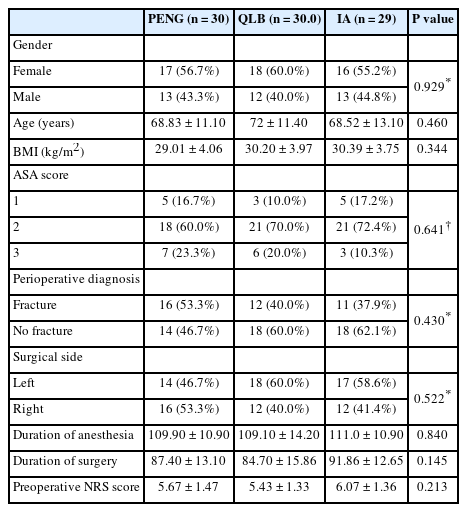
A total of 112 patients were screened, and 22 were excluded from the study. After completing randomization, one patient in the IA group was excluded because of unsuccessful spinal anesthesia. A total of 89 patients were thus analyzed: 30 in the PENG group, 30 in the QLB group, and 29 in the IA group (Fig. 3). The demographic and clinical characteristics of the study groups are shown in Table 1.
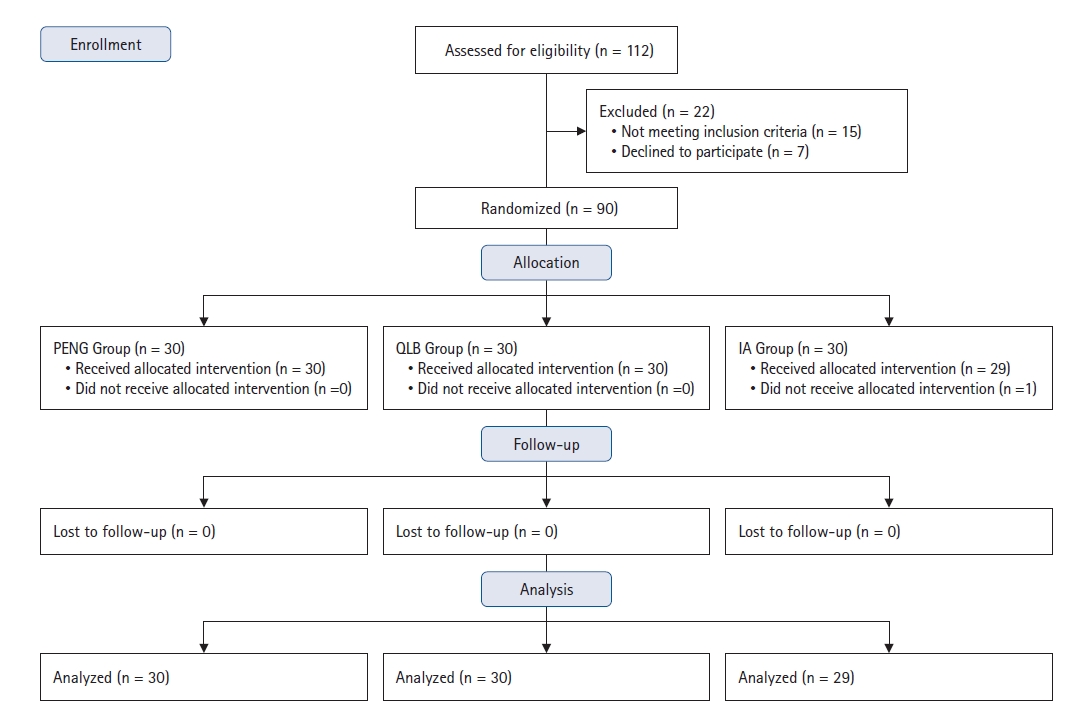
Consolidated Standards of Reporting Trials (CONSORT) flow diagram. PENG: pericapsular nerve group, QLB: quadratus lumborum block, IA: intra-articular injection.
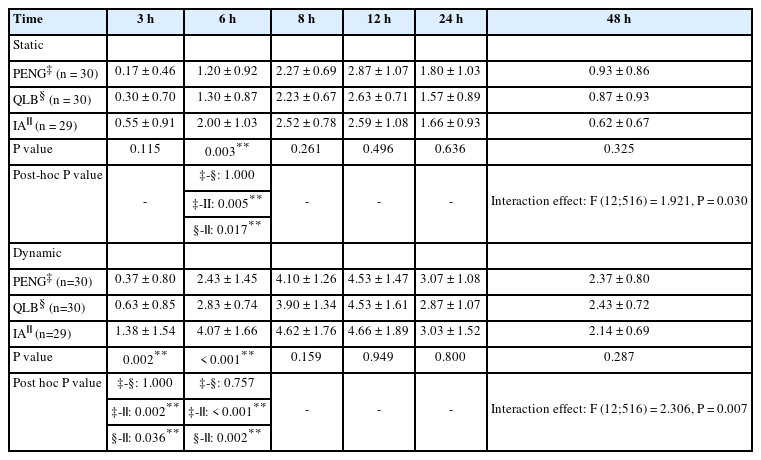
A comparison of the static and dynamic NRS scores between the groups is presented in Table 2. According to the post-hoc test results, the dynamic NRS scores of the PENG (0.37 ± 0.80) and QLB (0.63 ± 0.85) groups 3 h postoperatively were significantly lower from those of the IA (1.38 ± 1.54) group (P = 0.002, P = 0.036, respectively). Both the static and dynamic NRS scores of the IA group (static: 2.00 ± 1.03, dynamic: 4.07 ± 1.66) 6 h postoperatively were significantly higher from those of the PENG (static: 1.20 ± 0.92, dynamic: 2.43 ± 1.45; P = 0.005, P < 0.001, respectively) and QLB groups (static: 1.30 ± 0.87, dynamic: 2.83 ± 0.74; P = 0.017, P = 0.002, respectively) (Table 2). Intra- and inter-group comparisons of the static and dynamic NRS scores measured at the seven time points are presented in Supplementary Tables 1 and 2.
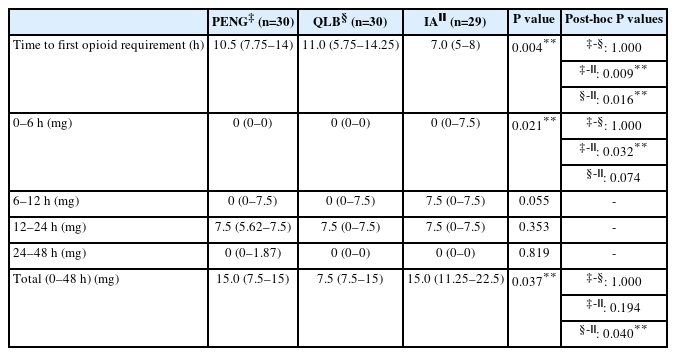
The post-hoc test results showed a significant difference in the time to first opioid requirement in the IA group compared to the PENG and QLB groups (7 [5, 8], 10.5 [7.75, 14], and 11 [5.75, 14.25]; P = 0.009 and P = 0.016, respectively). The analgesic requirement between 0 and 6 h in the PENG group was significantly different from that in the IA group (0 [0, 0] vs. 0 [0, 7.5]; P = 0.032). In the total time evaluated (0–48 h), only the amount of analgesic requirement in the IA group was significantly higher than that in the QLB group (7.5 [7.5, 15] and 15 [11.25, 22.5]; P = 0.040) (Table 3).
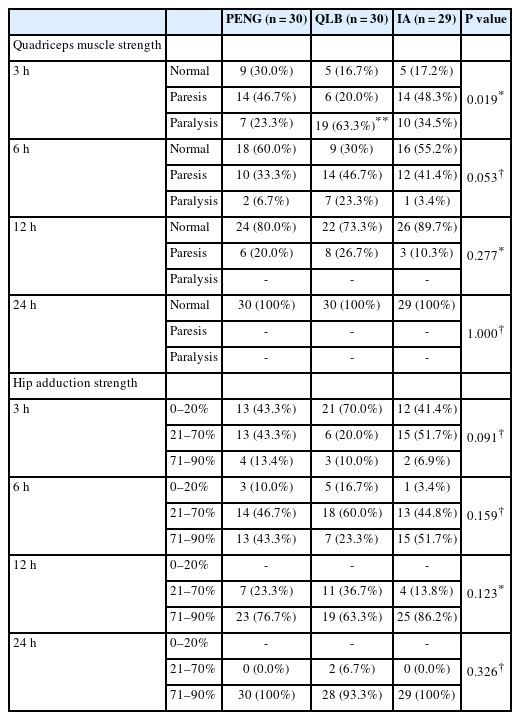
The distribution of the quadriceps muscle strength rates at 3 h was significantly different between the PENG (23.3%) and QLB (63.3%) groups (P = 0.019) (Table 4). According to the post-hoc test results, the quadriceps muscle strength at 3 h postoperatively in the QLB group was significantly lower than that in the PENG group (P = 0.007).
A statistically significant difference was observed in the time to mobilization between the study groups (P = 0.011) (Table 5). According to the post-hoc test results, the time to mobilization in the QLB group was significantly longer than that in the PENG group (17.3 ± 4.92 and 13.17 ± 4.43; P = 0.003). No significant differences were observed between the groups with respect to the QoR-40 score, patient satisfaction, or complications (Table 5).
Discussion
The results of this randomized controlled study demonstrated that the PENG block and QLB provided more effective analgesia for up to 6 h postoperatively than IA local anesthetic injections. QLBs and PENG blocks showed similar analgesic effects. The PENG block and QLB were more effective than the IA injection in terms of the time to first analgesia requirement. The PENG block was also found to be more effective at enabling early mobilization than the QLB, as it provided motor-protective analgesia up to 3 h postoperatively. Although the QLB had a similar effect to the PENG block with respect to 48-h opioid consumption, the QLB group was associated with less opioid consumption than the IA group. Despite the analgesic effects of the PENG block and QLB and the motor-protective effect of the PENG block, the three applications had a similar postoperative effect on the QoR.
Due to the complex innervation of the hip joint, the importance placed on regional anesthesia to provide adequate analgesia in THA is increasing. The presence of a large number of mechanoreceptors and nociceptors in the anterior capsule and innervation by the femoral and obturator nerves are the primary sources of pain in the hip joint [18]. Studies have shown that adequate analgesia is achieved with the PENG block as it effectively blocks the femoral, obturator, and accessory obturator nerves, which innervate the anterior capsule [16]. However, some studies have reported that the analgesic efficacy of PENG block for THA is limited and shown no evidence for the expected analgesic effect [14,19].
Cadaveric studies have found that the anterior QLB spreads to the lumbar plexus and paravertebral space, with wide dermatomal spread in the T7–L2 range [20]. Another recent cadaveric study showed that the anterior (transmuscular) QLB consistently spreads to the lumbar nerve roots and subcostal nerves compared with lateral QLB and posterior QLB [9]. Due to infiltration from the QLM and PM, spread of the QLB to the ilioinguinal, iliohypogastric, lateral cutaneous femoral nerves, genitofemoral nerve, and obturator nerves differs [21]. Another cadaveric study and case series demonstrated that the suprailiac approach to the anterior QLB includes T10–L3 dermatomal coverage [8]. Kukreja et al. [10] reported that the anterior QLB provided effective postoperative THA analgesia in the first 48 h postoperatively and reduced opioid consumption. In a study comparing the combination of the PENG block and QLB with the PENG block alone for hip revision surgeries, lower pain scores were observed in the combination group for the first 12–24 h [22].
These differing results for the QLB in cadaveric studies are due to the widespread area and the inability to predict the distribution pattern of local anesthesia. Furthermore, given the deep location of the QLM and the adjacent retroperitoneal and abdominal organs, the clinical use of the QLB is limited. Other factors that limit its use include the need for advanced technical skill and considerable attention to detail [20]. In the current study, both the QLB and PENG block provided similar analgesic effects, but the PENG block was more effective in terms of opioid consumption in the first 6 h postoperatively. Although the advantages of the PENG block include ease of implementation technically with patient positioning, the limited duration of analgesia for hip surgery may be a disadvantage.
As demonstrated in previous studies, administration of the PENG block [16], QLB [10], or IA injection [12,13] alone contributes to a reduction in postoperative pain scores and opioid consumption in patients undergoing THA. To the best of our knowledge, however, this is the first randomized controlled study to compare these three techniques. In a study by Pascarella et al. [16], the PENG block was found to significantly reduce the 48-h NRS values; however, as the intervention group could not be blinded, a strong postoperative evaluation could not be made. Another recent study emphasized that adding a PENG block to IA injection under general anesthesia does not contribute to the analgesic effect [19]. For the current study, spinal anesthesia was administered to limit high-dose opioid use intraoperatively. Opioid-induced hyperalgesia and opioid tolerance, which may occur following the use of short-acting opioids, were therefore avoided. The current study results showed that the PENG block significantly reduced NRS scores, and opioid consumption was lower at 6 h compared to IA local anesthetic injection.
Femoral, fascia iliaca, and epidural blocks cause delays in mobilization [23]. As a result, length of hospital stay is prolonged, and complications may develop. One recent study concluded that the motor-protective effect of the PENG block was superior to that of the suprainguinal fascia iliaca block [14]. Another study comparing the PENG and femoral blocks in patients with femoral fractures found that the PENG block was better at preserving quadriceps strength. However, it has also been shown that, because of the medial spread of a high amount of local anesthesia, the PENG block can cause obturator motor blockade [24]. Although the current study results showed that motor function was well preserved with the PENG block in the first 3 h postoperatively compared to the QLB, no difference was found at the other evaluation times. Given that patients undergoing the PENG block have a shorter time to mobilization, this block is more frequently preferred for early mobilization [14,25]. Additionally, unpredictable nerve root involvement may occur as a result of the QLB spreading in the fascial compartments and covering a wide network of nerves.
No difference was found among the three methods used in this study with respect to postoperative patient satisfaction or QoR scores. Earlier patient mobilization has been associated with fewer complications, lower mortality rates and pain scores, and shorter lengths of hospital stay [26,27]. Although the PENG block provided effective analgesia only at some of the evaluation points, the associated earlier mobilization increased clinicians’ preference for this block, especially in the fragile eldery patient group.
This study had some limitations. First, no normal control group was included. The presence of a control group is essential to evaluate the effectiveness of a given block. Nevertheless, data from previous studies showed that a sham or placebo group would be unlikely to change the clinical interpretation of these results. Although the study was planned to be prospective and randomized, the patients may not have been completely blinded because they were awake while the block was administered. However, based on the postoperative evaluation questions, the patients appeared to be unaware which block was performed. Finally, the use of drainage for psotoperative follow-up purposes during the surgical procedure was presumed to reduce the infiltration of bupivacaine into the surrounding tissue when administered as an IA injection.
In conclusion, the PENG block and QLB provided effective analgesia for up to 6 h postoperatively. The PENG block reduced opioid consumption during the first 6 h compared to IA local anesthetic injection. In addition, the motor-protective effect of the PENG block enabled earlier patient mobilization. However, similar results were obtained for the PENG block, QLB, and IA injection with respect to postoperative QoR.
Acknowledgements
The authors would like to offer special thanks to the Department of Anesthesia and Department of Orthopedics at Karaman Training and Research Hospital.
Notes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Tayfun Et (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing)
Muhammet Korkusuz (Methodology; Writing – original draft; Writing – review & editing)
Supplementary Materials
Intragroup and intergroup comparisons of NRS static and dynamic values measured at 7 different time points.
Comparison of NRS scores measured at static in study groups.
Comparison of NRS scores measured at movement in study groups.