Single-shot regional anesthesia for laparoscopic cholecystectomies: a systematic review and network meta-analysis
Article information
Abstract
Background
Different regional anesthesia (RA) techniques have been used for laparoscopic cholecystectomy (LC), but there is no consensus on their comparative effectiveness. Our objective was to evaluate the effect of RA techniques on patients undergoing LC using a network meta-analysis approach.
Methods
We conducted a systematic review and network meta-analysis. We searched PubMed, the Cochrane Central Register of Controlled Trials (CENTRAL), Scopus, and Web of Science (Science and Social Science Citation Index) using the following PICOS criteria: (P) adult patients undergoing LC; (I) any RA single-shot technique with injection of local anesthetics; (C) placebo or no intervention; (O) postoperative opioid consumption expressed as morphine milligram equivalents (MME), rest pain at 12 h and 24 h post-operation, postoperative nausea and vomiting (PONV), length of stay; and (S) randomized controlled trials.
Results
A total of 84 studies were included. With the exception of the rectus sheath block (P = 0.301), the RA techniques were superior to placebo at reducing opioid consumption. Regarding postoperative pain, the transversus abdominis plane (TAP) block (−1.80 on an 11-point pain scale) and erector spinae plane (ESP) block (−1.33 on an 11-point pain scale) were the most effective at 12 and 24 h. The TAP block was also associated with the greatest reduction in PONV.
Conclusions
RA techniques are effective at reducing intraoperative opioid use, postoperative pain, and PONV in patients undergoing LC. Patients benefit the most from the bilateral paravertebral, ESP, quadratus lumborum, and TAP blocks.
Introduction
Laparoscopic cholecystectomy (LC), the most frequently performed upper abdominal laparoscopic surgery, is the gold standard treatment modality for gallbladder disorders, such as cholelithiasis and cholecystitis [1,2]. This minimally invasive procedure is considered superior to open surgery, especially due in terms of lower postoperative pain and early recovery, and triggers a relatively reduced immune response [3,4].
Although LC is considered less painful than open surgery, postoperative pain must still be managed [5]. The components of pain in laparoscopic upper abdominal surgeries differ from those in open surgeries. Some of these components include incisional pain, visceral pain, pain secondary to peritoneal irritation, and shoulder pain [5,6]. Despite these many components, the primary source of pain reported for LC is incisional; therefore, incisional pain should be the main focus of postoperative pain management [5]. However, a multimodal analgesic approach that alleviates all components of pain is the most appropriate. Generally, multimodal analgesia is applied in LC, including regional anesthesia (RA) techniques. Some components of multimodal analgesia in LC include nonsteroidal anti-inflammatory drugs and paracetamol, opioids, local infiltration analgesia, fascial plane blocks, and paravertebral and peri-paravertebral blocks [2,7,8].
Many meta-analyses have evaluated different RA techniques for postoperative pain and analgesia requirements in LC [2,9–13]. Herein, we designed and conducted a systematic review and meta-analysis of all randomized controlled comparative studies that evaluated the effect of RA techniques, including infiltration, in LC. The primary outcome of this analysis was postoperative morphine consumption. In addition, this study aimed to compare the overall relative effectiveness of each technique.
Materials and Methods
The network meta-analysis protocol used for this study was registered prospectively (PROSPERO identification number: CRD42022307399), and we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Statement Guidelines in order to prepare the present manuscript [14].
Eligibility criteria
Studies were considered eligible for inclusion based on the following PICOS criteria: (P) surgical patients aged > 18 years requiring LCA; (I) any RA single-shot technique with local anesthetics; (C) placebo or no intervention; (O) postoperative opioid consumption expressed as morphine milligram equivalents (MME), rest pain at 12 and 24 h post-operation, postoperative nausea and vomiting (PONV), and hospital length of stay (LOS); and (S) randomized controlled trials.
Search strategy
We performed a systematic search of the medical literature for the identification, screening, and inclusion of articles. The search was performed in the following databases: PubMed, The Cochrane Central Register of Controlled Trials (CENTRAL), Scopus, and Web of Science (Science and Social Science Citation Index) from inception to April 9, 2022. We also performed literature snowballing by checking the references of the included studies to identify additional eligible studies. We did not apply any restrictions on the language, status, or year of publication. The search strategy used for each database is available as supplementary material (Supplementary Material 1, which reports our search strategy).
Study selection
Two researchers independently screened the titles and abstracts of the identified papers to select the relevant manuscripts. The full text of every citation considered potentially relevant was reviewed.
Data extraction and data retrieval
After identifying studies that met the inclusion criteria, two authors manually reviewed and assessed each of the included studies. Opioids were converted to compare intravenous MME using the GlobalRPh morphine equivalent calculator, considering a 0% cross-tolerance modifier (http://www.globalrph.com/narcotic).
Quality assessment and certainty of evidence assessment
Two team members independently evaluated the quality of the included RCTs using the Risk of Bias (RoB) 2 tool [15]. Disagreements were resolved through discussion, or, if the disagreement could not be resolved, a third researcher was consulted. According to the RoB 2 tool, the overall risk of bias is expressed using a three-grade scale (i.e., “low risk of bias,” “high risk of bias,” or “ some concerns”). We used the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach to assess the certainty of evidence related to each of the outcomes [16].
Statistical methods
The meta-analysis was performed using R version 4.1 (R Foundation for Statistical Computing, Austria) and the ‘netmeta’ package. The treatment effect on continuous outcomes was expressed as the mean difference (MD) with a 95% CI. The treatment effect for dichotomous outcomes was expressed as the odds ratio (OR) with a 95% CI. The methods were ranked based on the frequentist analog of the surface under the cumulative ranking curve [17]. When necessary, we converted the reported median and interquartile range to the estimated mean and SD using Hozo’s method [18]. We decided not to apply continuity correction to zero events.
Inconsistency, heterogeneity, and publication bias analysis
To assess study heterogeneity, the chi-square test and I2 statistic were used (I2 values were classified as follows: low, < 25%; moderate, 25–50%; and high, > 50%) [19]. The within-design heterogeneity and between-design inconsistency were evaluated using Cochrane Q. A random-effects model was preferred, regardless of both inconsistency and heterogeneity. Publication bias was evaluated by visual inspection of funnel plots.
Results
Study selection and data retrieval
The search results are shown in the PRISMA diagram (Fig. 1). The initial screening identified 9,124 studies. Of these, 8,955 were excluded during the preliminary screening because they were unrelated or duplicate studies. The remaining 169 full-text manuscripts were retrieved, 85 of which were excluded based on the inclusion and exclusion criteria. A total of 84 studies that evaluated nine different RA techniques were included in the quantitative and qualitative analyses [20–103].
The regional and local anesthesia techniques assessed included intraperitoneal local anesthetic instillations; wound/port infiltrations; and erector spinae plane (ESP), transversus abdominis plane (TAP), subcostal TAP, rectus sheath, quadratus lumborum (QL), and paravertebral blocks. The resulting network is shown graphically in Fig. 2.

Network graph. Overview of the network. Each regional anesthesia technique is represented at each corner of the polygon. The width of the lines connecting interventions are proportional to the number of trials assessing the comparisons. ESP: erector spinae plane, QL: quadratus lumborum, TAP: transversus abdominis plane.
According to the risk of bias evaluation, seven studies were classified as low risk of bias, ten as high risk of bias, and the remaining studies had some concerns (Fig. 3). The criteria used to assign these risk of bias judgments are available as supplementary material (Supplementary Material 2 with the risk of bias table).
Study characteristics
The 84 studies included a total of 6,214 patients. Of these, 2,079 were allocated to the placebo or no intervention groups, while 4,135 were allocated to the regional or local anesthesia groups (1,117 to wound/port infiltrations, 1,490 to intraperitoneal instillations, 263 to ESP blocks, 447 to TAP blocks, 520 to subcostal TAP blocks, 86 to rectus sheath blocks, 149 to QL blocks, and 63 to paravertebral blocks). Among the comparator groups, 70 studies used placebo/no intervention, 30 used wound/port infiltrations, 37 used intraperitoneal instillations, 8 used ESP blocks, 12 used TAP blocks, 15 used subcostal TAP blocks, 3 used rectus sheath blocks, 4 used QL blocks, and 2 used paravertebral blocks. The characteristics of all the included studies are available for consultation (Supplementary Material 3).
Outcomes
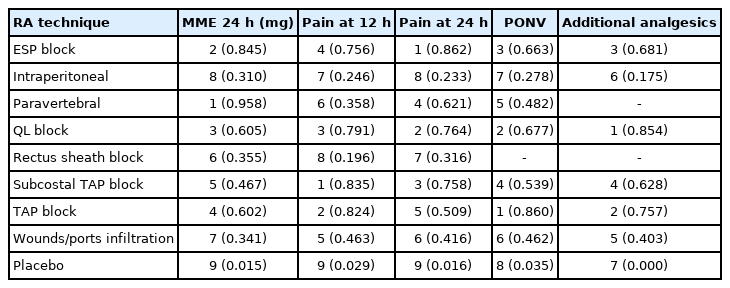
Primary outcome: postoperative opioid consumption at 24 h
Postoperative opioid consumption was evaluated in 46 of the studies. With the exception of the rectus sheath block (P = 0.301), all RA techniques were superior at reducing opioid consumption compared to placebo. The most effective block in our analysis was the paravertebral block (−6.64 MME [−9.67, −3.63]). The results for the primary outcome are graphically depicted in Fig. 4, and the results for all outcomes are summarized in Tables 1 and 2, and additionally, direct and indirect evidence contributing to each outcome is available as Supplementary Material 4.
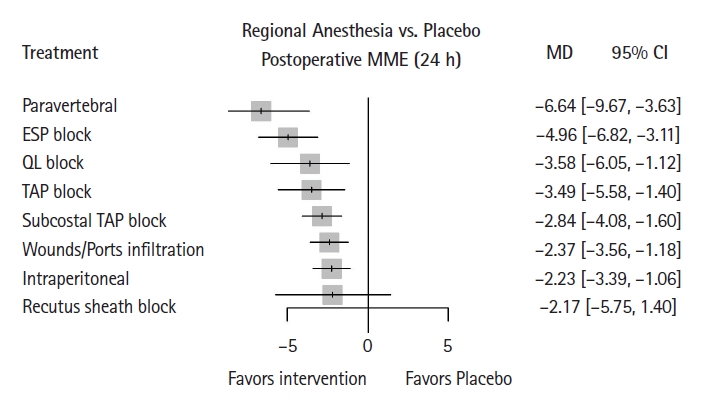
Forest plot of the network meta-analysis. Morphine consumption at 24 h expressed as MME. MME: morphine miligram equivalents, MD: mean difference, ESP: erector spinae plane, QL: quadratus lumborum, TAP: transversus abdominis plane.
Using the GRADE assessment, the quality of evidence was rated as low due to high heterogeneity (I2 = 96.6%) and evidence of possible publication bias according to the Egger test.
Postoperative pain at 12 h
Postoperative pain at 12 h was evaluated in 53 of the studies. Compared to placebo, the greatest reduction in pain was obtained with the subcostal TAP block (−1.80 [−2.21, −1.36] on an 11-point pain scale). Notably, the paravertebral block did not reach statistical significance given the relatively low sample size compared to the other interventions, resulting in a large CI (−1.92, 0.32).
Using the GRADE assessment, the quality of evidence was rated as moderate owing to high heterogeneity (I2 = 85.4%).
Postoperative pain at 24 h
Postoperative pain at 24 h was evaluated in 65 of the studies. The ESP block was associated with the greatest pain reduction compared to placebo (−1.33 [−1.96, −0.71] on an 11-point pain scale). Irrespective of the block type, the pain scores in the control groups were greater than those in the RA groups. For this outcome, the paravertebral block did not reach statistical significance, and had a large CI (−2.15, −0.15).
Using the GRADE assessment, the quality of evidence was rated as moderate owing to high heterogeneity (I2 = 89.6%).
PONV
PONV was evaluated in 40 of the studies. This outcome was not available for the rectus sheath block. The relevant studies assessing the ESP block, intraperitoneal instillation, TAP block, and wound/port infiltration resulted in a statistically significant reduction in PONV compared to placebo or no intervention. The highest reduction in PONV was obtained with the TAP block, with an OR of 0.35 (0.22, 0.57).
Using the GRADE assessment, the quality of evidence was rated as moderate with low heterogeneity (I2 = 0%), but high inconsistency.
Hospital length of stay
Only 12 of the studies evaluated the effect of RA on hospital length of stay. Considering the small number of trials, a meta-analysis was not performed to avoid potentially misleading results. We chose to provide a qualitative description of the results instead.
Three of the trials found a statistically significant difference, two of which investigated intraperitoneal instillation vs. placebo [56,97], while the third one evaluated ESP block vs. subcostal TAP block [65]. However, only one study found a difference that was both statistically and clinically significant [98] (1.3 ± 0.6 vs. 1.9 ± 1.2 days). For the other two trials, the mean difference was two [56] and three hours [65], respectively, which we considered clinically insignificant.
No differences in the hospital LOS were found in the remaining nine trials. These studies evaluated intraperitoneal instillation compared to placebo (five trials) [21,23,33,48,66], rectus sheath block compared to placebo (one trial) [67], paravertebral block compared to placebo (one trial) [73], wound/port infiltration compared to TAP block [90], and intraperitoneal instillation compared to TAP block compared to wound/port infiltration compared to placebo (one study) [24].
Use of rescue analgesics
The use of additional analgesics was also evaluated in 28 of the studies. All interventions were found to significantly reduced the use of postoperative rescue analgesics. The QL block was the most effective intervention, with an OR of 0.07 (95% CI [0.01, 0.40]).
Using the GRADE assessment, the quality of evidence was rated as moderate owing to high heterogeneity (I2 = 61.7%).
Publication bias
Egger’s test revealed a potential publication bias only for postoperative opioid consumption (P = 0.417). The funnel plots are available as Supplementary Material 5.
Sensitivity analysis
We performed a sensitivity analysis by removing studies with a high risk of bias. The results of the sensitivity analysis were not significantly different from the main analysis, moreover, such sensitivity analysis could not explain the possible publication bias for postoperative opioid consumption (Supplementary Material 6).
Discussion
Our study showed that patients receiving RA for LC had lower opioid consumption and pain in the first 24 h post-operation compared to placebo or no intervention. However, the limited amount of data prevented any conclusions regarding possible benefits to be made for hospital stay. LC is the most frequently performed upper abdominal laparoscopic surgery, and the 2018 PROSPECT guidelines for LC recommended that wound/port infiltration be the routine regional technique used; the other techniques were not recommended because of limited small trial evidence and the potential for complications or failure of the anesthetic technique [104]. However, in the four years since these guidelines were published, many studies have substantially improved our knowledge on this topic.
Pain after LC may be associated with both visceral and somatic innervation. Postoperative analgesia should therefore be chosen considering both sources of pain. Our analysis confirms that most RA techniques are effective at reducing postoperative opioid consumption, pain on the first postoperative day, and PONV, that all of which are in line with previously published guidelines [104].
Considering our primary outcome, the paravertebral block was the most effective technique with the most significant reduction in morphine consumption (6.64 mg). While this difference is statistically significant, previous studies have suggested that a reduction in morphine that is < 10 mg may have a limited clinical impact [105]. While the clinical significance of small reductions in opioid consumption has not been clearly established, a recent review showed that there are no clear data to define the minimal clinically important difference for 24 h opioid consumption [106].
Pain at 12 and 24 h post-operation similarly showed that most RA techniques were effective, with the subcostal TAP block and the ESP block showing the greatest effect. Among the RA techniques, only the paravertebral block did not show statistically significant results regarding pain in the first 24 h post-operation. This result is likely due to the relatively small sample size for the paravertebral block compared with the other interventions, that producinge a large CI.
Of note, while the small reduction in opioid consumption may be debatable, the overall benefit of these blocks on pain scores and PONV indicates that the benefits are not limited only to opioid consumption, but also affect overall patient comfort, strongly suggesting that these techniques should be routinely adopted.
Not all the investigated techniques appeared to be equally effective at achieving the desired results for morphine consumption or postoperative pain. In particular, the rectus sheath block was not statistically significant for any of the investigated outcomes, and intraperitoneal instillation of local anesthetics and wound/port infiltration were consistently among the least effective treatments. A recent meta-analysis investigating the effect of the rectus sheath block on various laparoscopic surgeries [13] found that the technique was effectively reduced pain for both the second and the composite –10–12 h post-operation, though it was not effective at 24 h post-operation. A limitation of this study relates to the inclusion of several different types of laparoscopic procedures, the majority of which are gynecological interventions. While we did not investigate early postoperative pain at 2 h, the evaluation of a single type of intervention makes our patient population more homogenous, potentially strengthening the significance of our results. Another potential limitation related to the use of the rectus sheath block in LC is that it targets only the anterior ramus of the ventral branch of the spinal nerve, which limits its ability to affect both visceral and abdominal wall pain originating from laparoscopic ports lateral to the rectus sheaths after LC. Previous studies have reported that visceral pain is the most significant contributor to pain in the first 24 h after LC [107,108]. Given this context, our results regarding the rectus sheath block were unsurprising.
Future studies comparing paravertebral and interfascial blocks are warranted. Moreover, considering that part of the evidence produced by our study arose from indirect evidence, more studies directly comparing interventions are necessary.
Our study has some limitations. First, all our analyses were characterized by high heterogeneity, likely resulting from the pooling of heterogeneous studies of anesthetic and analgesic regimens, which, if these characteristics interacted with the outcomes of the local anesthetic injection, may have compromised the estimated outcomes. Therefore, readers should be cautious when extrapolating and applying these results to routine clinical practice. Second, we pooled no-intervention and placebo groups together for the meta-analysis; however, no block is not the same as a placebo since it has no potential favorable psychological advantages. Placebo may cause a psychological effect lowering pain scores and opioid use when a patient is not offered a block in daily clinical practice. Analyzing these interventions individually improves the accuracy and strength of our results. Third, the conclusions regarding some RA techniques (such as the paravertebral block) were based on a small sample size, which greatly decreases the strength of the evidence for these techniques. While we decided not to remove these techniques from our analysis, further studies are necessary to increase the certainty of evidence regarding these blocks.
In conclusion, regional single-shot techniques are effective at reducing intraoperative morphine consumption, pain, and PONV in patients undergoing LC. Patients benefit the most from the bilateral paravertebral, ESP, QL, and TAP blocks. The rectus sheath block was not effective for the considered outcomes.
Notes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Alessandro De Cassai (Conceptualization; Data curation; Formal analysis; Methodology; Project administration; Writing – original draft; Writing – review & editing)
Nicolò Sella (Conceptualization; Data curation; Methodology; Writing – original draft; Writing – review & editing)
Federico Geraldini (Conceptualization; Methodology; Writing – original draft; Writing – review & editing)
Serkan Tulgar (Data curation; Methodology; Writing – original draft; Writing – review & editing)
Ali Ahiskalioglu (Investigation; Validation; Writing – original draft; Writing – review & editing)
Burhan Dost (Investigation; Visualization; Writing – original draft; Writing – review & editing)
Silvia Manfrin (Investigation; Writing – review & editing)
Yunus Emre Karapinar (Investigation; Writing – review & editing)
Greta Paganini (Investigation; Writing – review & editing)
Muzeyyen Beldagli (Investigation; Writing – review & editing)
Vittoria Luoni (Investigation; Writing – review & editing)
Busra Burcu Kucuk Ordulu (Investigation; Writing – review & editing)
Annalisa Boscolo (Methodology; Project administration; Supervision; Writing – original draft; Writing – review & editing)
Paolo Navalesi (Methodology; Project administration; Supervision; Writing – original draft; Writing – review & editing)
Supplementary Materials
Search Strategy.
Risk of Bias.
Study characteristics.
Direct and indirect evidence.
Funnel Plots.
Sensitivity analysis.