 |
 |
| Korean J Anesthesiol > Volume 75(3); 2022 > Article |
|
Abstract
Background
Prompt insertion and placement of supraglottic airway (SGA) devices in the correct position are required to secure the airway. This meta-analysis was performed to validate the usefulness of the 90° rotation technique as compared with the standard digit-based technique for the insertion of SGA devices in anesthetized patients in terms of insertion success rate, insertion time, and postoperative complications.
Methods
A literature search of PubMed, EMBASE, CENTRAL, CINAHL, Scopus, and Web of Science was conducted. Randomized controlled trials, without limitations on publication period, language, journal, or region, until July 2021, that compared the 90° rotation and the standard digit-based techniques for insertion of SGA devices in anesthetized patients were included.
Results
The first-attempt (risk ratio [RR]: 1.16, 95% CI [1.09, 1.25], P < 0.001) and overall success rates (RR: 1.06, 95% CI [1.03, 1.09], P < 0.001) were significantly higher in the 90° rotation group. The insertion time was shorter in the 90° rotation group (mean difference: −4.42 s, 95% CI [−6.70, −2.15 s], P < 0.001). The incidences of postoperative sore throat (RR: 0.63, 95% CI [0.49, 0.83], P < 0.001) and blood staining (RR: 0.28, 95% CI [0.20, 0.39], P < 0.001) were lower in the 90° rotation group.
Supraglottic airway (SGA) devices have increasingly been used to maintain the airway during anesthesia. The American Society of Anesthesiologists has recommended the use of SGA devices in the practice guidelines for management of difficult airways [1,2]. Various SGA devices have been developed and introduced, such as the ClassicTM laryngeal mask airway (LMA) (Laryngeal Mask Airway Co. Ltd., UK), ProsealTM LMA (Laryngeal Mask Co. Ltd., Seychelles), LMA flexibleTM (Teleflex Co., Ireland), and i-gelTM (Intersurgical, UK).
Prompt insertion and placement of the SGA device in the correct position are important during induction of anesthesia or emergency airway management. Conventionally, the standard digit-based technique involves using the index finger for SGA device insertion. However, this technique is somewhat difficult [3], and thus it requires certain training and some degree of skill [4]. Consequently, standard digit-based technique does not always ensure successful insertion and optimal placement of the SGA device. The first-attempt success rate of standard digit-based technique is reported to be 67–90% [5,6].
Various techniques have been investigated to increase the success rate of SGA device insertion in the first attempt, including the 90° rotation technique, 180° rotation technique, head elevation, or rotation and guidance technique [7–12]. Among these approaches, the 90° rotation technique was first introduced by Hwang et al. [7] in 2009. Thereafter, this technique has been investigated with a variety of SGA devices in several studies [8,11–13]. The 90° rotation technique has shown favorable results in increasing the success rate of SGA device insertion in several studies [8,12]. In contrast, it was unclear whether the 90° rotation technique could improve the success rate of SGA insertion compared to the standard digit-based technique [11,13].
Given the conflicting reports of previous studies, this meta-analysis was designed to verify the superiority of the 90° rotation technique over the standard digit-based technique in terms of insertion success rate and postoperative complications in anesthetized patients undergoing surgery.
This study was performed in accordance with the Preferred Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines [14]. The protocol was registered in the International Prospective Register of Systematic Reviews (CRD42021271253). In this study, we searched studies comparing the 90° rotation and the standard digit-based techniques for the insertion of SGA devices in patients undergoing general anesthesia. Eligible studies published until July 26, 2021, were searched on electronic databases, such as PubMed, EMBASE, CENTRAL, CINAHL, Scopus, and Web of Science. The search terms consisted of Medical Subject Headings (MeSH) terms and keywords, such as ‘Laryngeal Masks,’ ‘laryngeal mask,’ ‘LMA,’ or ‘rotation.’ Terms were combined with the Boolean operators ‘AND’ or ‘OR.’ The detailed search strategies for each database are shown in Supplemental digital content 1. The search was conducted without limitations on publication period, language, journal, or region.
Two authors (C.-H.K. and J.-H.R.) independently screened papers and selected eligible studies according to predefined inclusion and exclusion criteria. The inclusion criteria were: (1) randomized controlled trials (RCTs), (2) studies including patients with SGA device insertion under general anesthesia, (3) studies comparing the 90° rotation technique with the standard digit-based technique for insertion of the SGA device, (4) studies reporting outcomes regarding insertion success rate and complication rate. Exclusion criteria were: (1) animal studies, (2) non-randomized studies (e.g., observational studies, retrospective studies, or case reports), (3) incomplete papers (e.g., conference abstracts, protocols, letters, or editorials). The results obtained by searching each database were combined, and the title and abstract of each paper was examined to screen for relevant studies. Subsequently, we found and reviewed the full text of the relevant studies and included RCTs that met the inclusion criteria in the final analysis. If any disagreement occurred during study selection, a third author (J.-W.H.) participated in the study selection and made the final decision.
The RCTs included in the final analysis were reviewed, and data were extracted and summarized into Excel sheets (Microsoft Inc., USA). The data extracted were the following: (1) name of the first author, (2) publication year, (3) sample size, (4) age of participants, (5) type and size of SGA device, (6) cuff pressure of SGA device before insertion, (7) allowance of manipulation during SGA device insertion, (8) types of neuromuscular blocking agents (NMBA) used, (9) success rates for SGA device insertion, (10) insertion time, and (11) postoperative complications regarding SGA device placement. If the result in a study was only plotted as a graph, we extracted the numerical data using the GetData Graph Digitizer 2.26 (http://www.getdata-graph-digitizer.com). The primary outcome was the first-attempt success rate for SGA device insertion. Secondary outcomes included the overall success rate for insertion, insertion time, and postoperative complications regarding SGA device insertion. The definitions of success of SGA placement and insertion time in each RCT are summarized in Supplemental digital content 2. Complications were defined as postoperative sore throat and pharyngeal injury assessed by blood stains on the surface of the SGA device.
The risk-of-bias (RoB) of each RCT was assessed using the revised Cochrane RoB tool (RoB 2) [15]. Two authors (C.-H.K. and J.-H.R.) independently reviewed the full text of each RCT and graded the level of the RoB. The RoB 2 has five domains (randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result) and each domain is graded as ‘low risk,’ ‘some concerns,’ or ‘high risk.’ Subsequently, the overall RoB in each RCT was determined according to the RoB for each domain. When all domains were graded ‘low risk,’ the overall RoB was considered ‘low risk.’ If there were ‘some concerns’ without ‘high risk,’ the overall RoB was determined to be ‘some concerns.’ If at least one domain was graded ‘high risk,’ the overall RoB was considered ‘high risk.’ Any disagreements were resolved by participation of the third author (Y.-T.J.).
The level of evidence for each outcome was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system [16]. It has five domains including RoB, inconsistency, indirectness, imprecision, and publication bias.
To determine the degree of agreement between two authors for the study selection and data extraction, we calculated the kappa value and interpreted the value as follows according to the Cochrane Handbook [17]: 0.4–0.59, fair agreement; 0.6–0.75, good agreement; 0.75–1.0, excellent agreement.
We used R statistical software version 3.6.1. (R Foundation for Statistical Computing, Austria) with the ‘meta’ and ‘metafor’ package to conduct data synthesis and meta-analyses [18–20]. We calculated the risk ratio (RR) for categorical variables, such as success rates and the incidence of postoperative complications. We calculated the mean differences (MDs) for the insertion time (a continuous variable). In addition, sensitivity analysis was performed by using the leave-one-out approach to assess the robustness of our findings. The level of heterogeneity across studies was determined by calculating the inconsistency index (I2). If I2 < 50%, a fixed-effects model was used; otherwise, a random-effects model was used to estimate effect size. To explore the potential sources of heterogeneity, we planned to perform subgroup analysis according to the age of participants (adults vs. children), use of NMBAs, allowance of manipulation during SGA device placement, and cuff pressure before insertion. Additionally, we also conducted meta-regression analysis in case significant heterogeneity was observed. All subgroup-, sensitivity-, and meta-regression analyses were restricted to the primary outcome. We constructed funnel plots and conducted Egger’s linear regression analysis to detect publication bias. A P value < 0.05 was considered statistically significant.
The literature search yielded 589 papers, of which 300 were duplicate. The remaining 289 papers were screened, and of these, 275 irrelevant papers were excluded. A review of the remaining 14 papers led to the exclusion of four papers based on the exclusion criteria: incomplete papers (n = 3) and a non-randomized study design (n = 1). Therefore, 10 RCTs, with 1,286 patients, were included in the final meta-analysis (Fig. 1) [7,8,11–13,21–25]. In the study selection, the kappa value between two authors was 0.811, indicating excellent agreement.
Among the participants, 644 patients were allocated to the 90° rotation group and 642 patients were allocated to the standard group. The characteristics of each RCT are shown in Table 1. Since nine of the 10 RCTs included adult patients, we decided not to conduct subgroup analysis according to age. The ProsealTM LMA device was used in half of the included RCTs [7,8,12,22,24] and the i-gelTM device was used in two RCTs [21,25]. The ClassicTM, UniqueTM, and FlexibleTM LMA devices were placed in the remaining RCTs [11,13,23]. In six RCTs, the SGA cuff was fully deflated before insertion and was inflated after placement [7,8,11–13,24]. The cuff was partially inflated before insertion in another two RCTs [22,23]. The remaining two RCTs employed the i-gelTM, which has no cuff [21,25]. In six RCTs, authors performed manipulations, including chin lift, jaw thrust, head extension, neck flexion, or movement of the SGA device for device placement, if needed [7,11,13,21,24,25]. NMBAs were administered before SGA device insertion in seven RCTs [8,11–13,21,24,25], whereas no NMBA was used in three RCTs [7,22,23]. In terms of interrater reliability for data extraction, the kappa value was 0.759 that indicated excellent agreement between two authors.
We extracted or estimated the first-attempt success rate for SGA device insertion in all 10 RCTs [7,8,11–13,21–25]. The SGA device was placed properly in the first attempt in 612 patients (95.0%) in the 90° rotation group and in 522 patients (81.3%) in the standard group. Hence, the first-attempt success rate was significantly higher in the 90° rotation group than in the standard group (RR: 1.16, 95% CI [1.09, 1.25], P < 0.001, I2 69%; random-effects model; Fig. 2A). Sensitivity analysis showed that the RR remained stable, implying that no single RCT skewed the pooled effect size (Supplemental digital content 3). In the subgroup analyses (Supplemental digital content 4), the RRs remained stable in NMBA (studies = 7, RR: 1.12, 95% CI [1.04, 1.22], P = 0.004) no NMBA (studies = 3, RR: 1.27, 95% CI [1.11, 1.44], P < 0.001), manipulation (studies = 6, RR: 1.10, 95% CI [1.02, 1.18], P = 0.008), no manipulation (studies = 4, RR: 1.30, 95% CI [1.18, 1.43], P < 0.001), no cuff (studies = 2, RR: 1.11, 95% CI [1.02, 1.20], P = 0.016), inflated cuff (studies = 2, RR: 1.35, 95% CI [1.13, 1.61], P = 0.001), and deflated cuff (studies = 6, RR: 1.15, 95% CI [1.05, 1.25], P = 0.003) subgroups. Meta-regression analysis showed that allowing manipulation during SGA device insertion had a significant influence on the pooled effect size (P = 0.005), accounting for the considerable level of heterogeneity (53.03%) (Supplemental digital content 5). The funnel plot is shown in Supplemental digital content 6. Egger’s linear regression analysis revealed that publication bias was insignificant (P = 0.300).
The overall success rate was reported in seven RCTs, with a total of 917 patients [7,8,12,21,23–25]. It was 98.7% in the 90° rotation group and 93.0% in the standard group. An RR of 1.06 indicated that the 90° rotation technique significantly improved the overall success rate of SGA device insertion as compared to the standard technique RR: 1.06, 95% CI [1.03, 1.09], P < 0.001, I2 0%, fixed-effects model; Fig. 2B). The funnel plot is shown in Supplemental digital content 7. The results of Egger’s linear regression analysis proved that there was no significant publication bias (P = 0.662).
Insertion time was reported in all 10 RCTs [7,8,11–13,21–25]. Mahmoodpoor et al. [23] showed the time for SGA device insertion as a graph, and the unit of time in the figure was ‘minutes.’ However, according to the main text of their paper, the unit of time was ‘seconds.’ We contacted the study author and confirmed that the unit of time was ‘seconds.’ In addition, we regarded that the error bar represented the standard error of mean. The results of our meta-analysis demonstrated that the 90° rotation technique required less time for SGA device placement than the standard technique (MD: −4.42 s, 95% CI [−6.70, −2.15] s, P < 0.001, I2 91%, random-effects model; Fig. 3). The funnel plot is shown in Supplemental digital content 8. The results of Egger’s linear regression analysis confirmed that there was no significant publication bias (P = 0.173).
Postoperative sore throat was reported in nine RCTs [7,8,11–13,21,22,24,25]. A total of 75 patients (12.7%) in the 90° rotation group experienced sore throat after surgery, while 118 patients (20.1%) in the standard group experienced sore throat after surgery. The meta-analysis confirmed that fewer patients in the 90° rotation group had postoperative sore throat than those in the standard group (RR: 0.63, 95% CI [0.49, 0.83], P < 0.001, I2 47%, fixed-effects model; Fig. 4A).
Blood staining on the SGA device surface was reported in all 10 RCTs [7,8,11–13,21–25]. The incidence of blood staining was 6.2% in the 90° rotation group and 22.3% in the standard group. An RR of 0.28 implied that the 90° rotation technique significantly decreased the incidence of blood staining on the SGA device surface as compared to the standard technique (RR: 0.28, 95% CI [0.20, 0.39], P < 0.001, I2 17%, fixed-effects model; Fig. 4B).
Given the symmetrical funnel plots and results of Egger’s linear regression analysis of funnel plot asymmetry (P = 0.968 and 0.806, respectively), publication biases for postoperative complications were considered insignificant (Supplemental digital content 9).
As shown in Supplemental digital content 10, the overall RoB was rated as ‘low risk’ in four RCTs and ‘some concerns’ in five RCTs. The reason for ‘some concerns’ was the absence of descriptions of allocation concealment [4,10,16–18,20]. Due to the design of the studies, it was impossible to blind the anesthesiologists who inserted the SGA device in all studies. However, objective approaches, for example, a square wave of capnograph or a blinded observer were used to determine the success rate of SGA insertion. Therefore, we judged that the awareness of the allocated group may not have affected the assessment of outcome.
The level of evidence for each outcome was shown in Supplemental digital content 11. The level of evidence was moderate for first-attempt success rate and postoperative complications, high for overall success rate, and low for insertion time.
The present meta-analysis showed that the 90° rotation technique increased both the first-attempt success and overall success rate as compared to the standard digit-based technique during the insertion of SGA devices in anesthetized patients. The 90° rotation technique also reduced SGA device insertion time. In addition, it was associated with less postoperative complications, in that the incidence of postoperative sore throat and mucosal bleeding was lower in patients intubated using the 90° rotation technique than in those intubated with the standard digit-based technique.
Insertion success rate is the most critical outcome in terms of SGA device insertion. The 90° rotation technique increased both the first attempt and overall success rate as compared with the standard digit-based technique in anesthetized adults (nine studies) and children (one study). These results correlate fairly well with a previous study and further support the role of the 90° rotation technique in SGA device insertion. Park et al. [26] conducted meta-analysis with 13 RCTs and concluded that rotation technique provided higher first-attempt and overall success rate. However, they included both 90° and 180° rotation techniques. Among the included studies, there are only four studies that compared the 90° rotation to standard technique. Given that our results are based on more RCTs that validated the 90° rotation technique solely, our study may provide further evidence for the usefulness of the 90° rotation technique. During the advancement of the SGA device by means of the standard digit-based technique, impaction and friction at the back of the mouth are often encountered, which are the main causes of failed insertion [27]. Furthermore, some types of SGA device have soft bowl, large cuff, or flexible shaft [28,29]. These features may disturb the insertion of the SGA device. In the 90° rotation technique, the SGA device is inserted until the cuff is inside the mouth; then, it is rotated 90° and advanced until resistance from the hypopharynx is felt; and finally, it is straightened out in the hypopharynx [7]. Therefore, the 90° rotation technique may reduce the resistance between the SGA and the posterior pharyngeal wall at the lateral edge of the oral cavity, making advancement of the SGA device easier. The reduced insertion time of the 90° rotation technique may be explained by the same oral cavity anatomical factors mentioned above.
This meta-analysis included studies that used various SGA devices including the ClassicTM, ProsealTM, FlexibleTM, UniqueTM, and i-gelTM devices. Hence, a moderate degree of heterogeneity may be shown for the first-attempt success rate. We performed subgroup, sensitivity, and meta-regression analyses to explore the potential sources of heterogeneity. We found that the allowance for manipulations of SGA device insertion accounted for the heterogeneity. It is reasonable to infer that manipulation could facilitate SGA device insertion and affect the success rate. It is notable in this study that the 90° rotation technique improved the first-attempt success rate for device placement, irrespective of whether NMBA was administered, whether manipulation for placement was allowed, or whether the cuff was inflated or deflated. We believe that the results of subgroup analyses emphasize the validity of the 90° rotation technique in various circumstances. There was a high degree of heterogeneity in the insertion time. We recognized that definitions of success and insertion time were slightly inconsistent among the studies, and that these discrepancies might cause heterogeneity in the first-attempt success rate and insertion time. Nevertheless, it is interesting to note that there was no heterogeneity in the overall success rate.
Postoperative complications related to SGA device insertion results in postoperative sore throat and mucosal bleeding, which is manifested by blood staining on the surface of the removed SGA device. The 90° rotation technique was associated with a significantly reduced incidence of sore throat and mucosal bleeding as compared with the standard digit-based technique. This result may also be due to the reduced resistance and friction between the shaft of the SGA and the pharyngeal wall at the lateral edge of the oral cavity [7].
This study had several limitations. First, generally, SGA insertion requires certain training and sufficient experience. The SGA could be skillfully inserted only after mastering the correct method. Therefore, the professional title and experience of the researcher may be important factors for the success rate of SGA placement. Second, this study included electively anesthetized patients, and thus, it is difficult to extrapolate our findings to other fields, such as the emergency department. Third, RCTs included in this study used five types of SGA devices. However, there are various types of SGA devices which are not included in this study, for example, Softseal LMA. Given that our findings are based on five types of SGA devices, the results from this analysis should be treated with caution and are hardly to be generalized to all types of SGA devices.
In conclusion, this meta-analysis of 10 RCTs demonstrated that the 90° rotation technique was superior to the standard digit-based technique during insertion of the SGA device in anesthetized patients in that it was associated with increased first-attempt and overall success rate of device insertion, decreased insertion time, and decreased postoperative complications than the standard digit-based technique. Further research is needed in un-anesthetized patients with difficult airways in emergency airway management situations.
NOTES
Author Contributions
Chang-Hoon Koo (Data curation; Investigation; Methodology; Software; Visualization; Writing – original draft)
Ah-Young Oh (Conceptualization; Investigation; Methodology; Visualization; Writing – original draft)
Young-Tae Jeon (Conceptualization; Investigation; Methodology; Resources; Writing – review & editing)
Jung-Won Hwang (Conceptualization; Investigation; Methodology; Resources; Validation; Writing – review & editing)
Jung-Hee Ryu (Conceptualization; Formal analysis; Investigation; Methodology; Supervision; Writing – review & editing)
Supplementary Materials
Supplementary Digital Content 2.
Definitions of success and insertion time for supraglottic airway (SGA) device placement in each study.
Supplementary Digital Content 3.
Forest plot for sensitivity analysis for first-attempt success rate. Omitting each study in turn did not skew the pooled effect size.
Supplementary Digital Content 4.
Forest plots for subgroup analyses of first-attempt success rate. Subgroup analysis was performed according to (A) the use of neuromuscular blocking agents (NMBA), (B) allowance for manipulation of supraglottic airway (SGA) placement, and (C) cuff pressure before insertion. The first-attempt success rate remained significantly higher in the 90° rotation group than in the standard group in the NMBA (P = 0.004), no NMBA (P < 0.001), manipulation (P = 0.008), no manipulation (P < 0.001), no cuff (P = 0.016), inflated cuff (P = 0.001), and deflated cuff (P = 0.003) subgroups.
Supplementary Digital Content 5.
Meta-regression analysis for the potential sources of heterogeneity.
Supplementary Digital Content 6.
Funnel plot for first-attempt success rate. Egger’s linear regression analysis of the funnel plot asymmetry revealed that publication bias was insignificant (P = 0.300).
Supplementary Digital Content 7.
Funnel plot for overall success rate. Egger’s linear regression analysis of the funnel plot asymmetry revealed that publication bias was insignificant (P = 0.662).
Supplementary Digital Content 8.
Funnel plot for insertion time. Egger’s linear regression analysis of the funnel plot asymmetry revealed that publication bias was insignificant (P = 0.173).
Supplementary Digital Content 9.
Funnel plots for postoperative complications. (A) Postoperative sore throat, (B) Blood staining on supraglottic airway (SGA) device surface. Egger’s linear regression analysis of the funnel plot asymmetry revealed that publication bias was insignificant (P = 0.968, 0.806, respectively).
Supplementary Digital Content 10.
Risk-of-bias graph. D1: bias arising from the randomization process, D2: bias due to deviations from the intended intervention, D3: bias due to missing outcome data, D4: bias in measurement of the outcome, D5: bias in the selection of the reported results. Green circle: low risk, yellow circle: some concerns.
Fig. 1.
PRISMA flow diagram for the included and excluded studies. A total of 589 papers were searched through databases. We excluded 300 duplicate papers and 275 irrelevant papers. The full texts of 14 eligible studies were reviewed, and four studies were excluded. Finally, a total of 10 RCTs were included in the final analysis. RCT: randomized controlled trial.
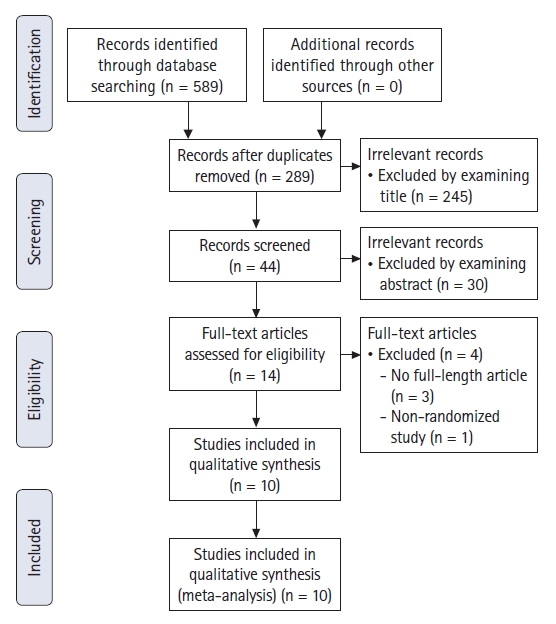
Fig. 2.
Forest plots for success rates of SGA insertion. (A) First attempt success rate, (B) overall success rate. Both first attempt success rate and overall success rate were significantly higher in the 90° rotation group than in the standard group (P < 0.001, respectively). SGA: supraglottic airway, RR: risk ratio.
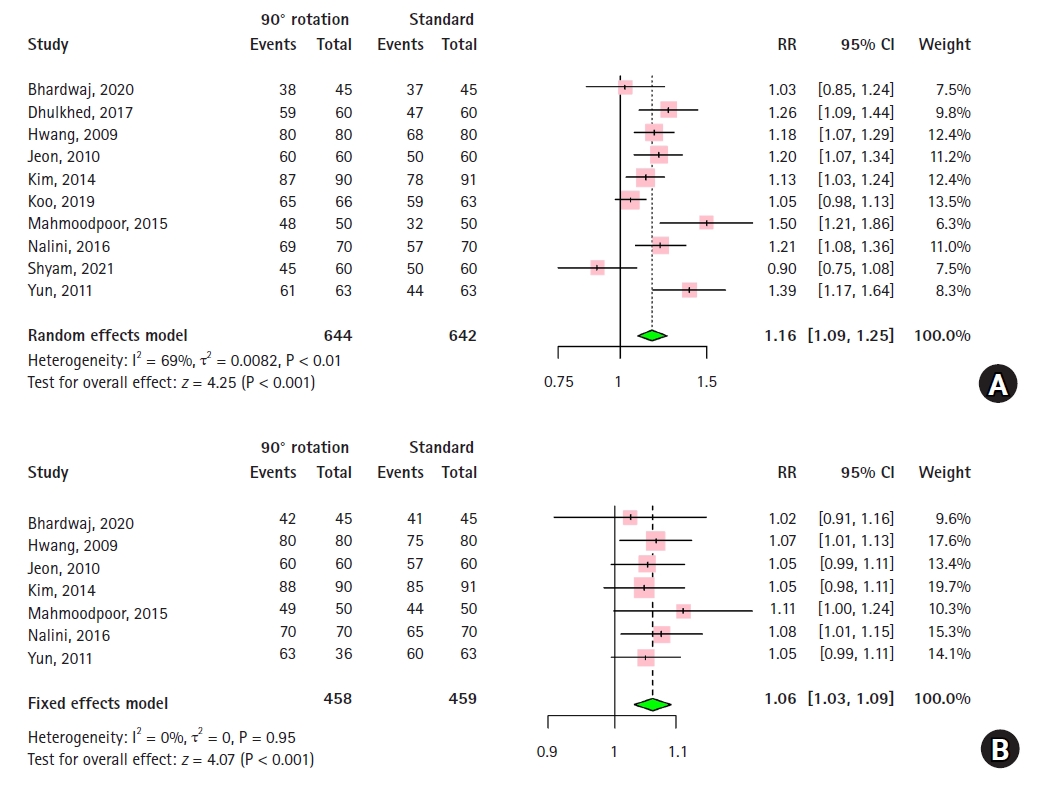
Fig. 3.
Forest plot for insertion time for SGA insertion. Insertion time was significantly lower in the 90° rotation group than in the standard group (P < 0.001). SGA: supraglottic airway, MD: mean difference, SD: standard deviation.
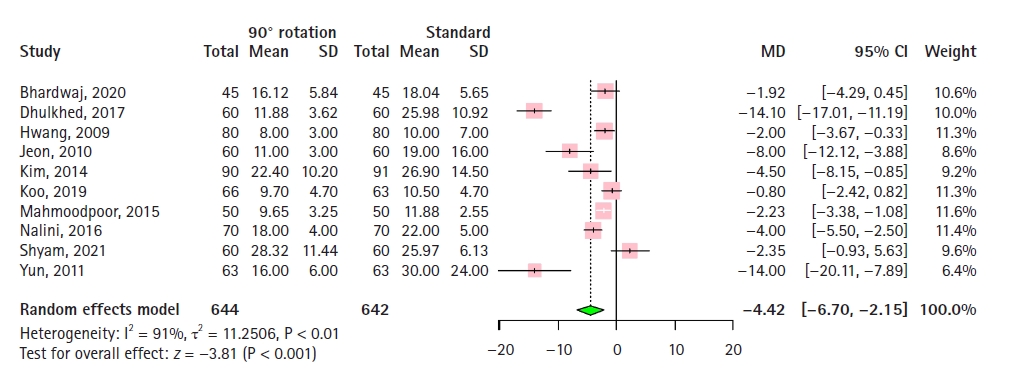
Fig. 4.
Forest plots for postoperative complications. (A) postoperative sore throat, (B) blood staining. The 90° rotation technique was associated with a significantly decreased incidence of postoperative sore throat and blood staining (P < 0.001, respectively). RR: risk ratio.
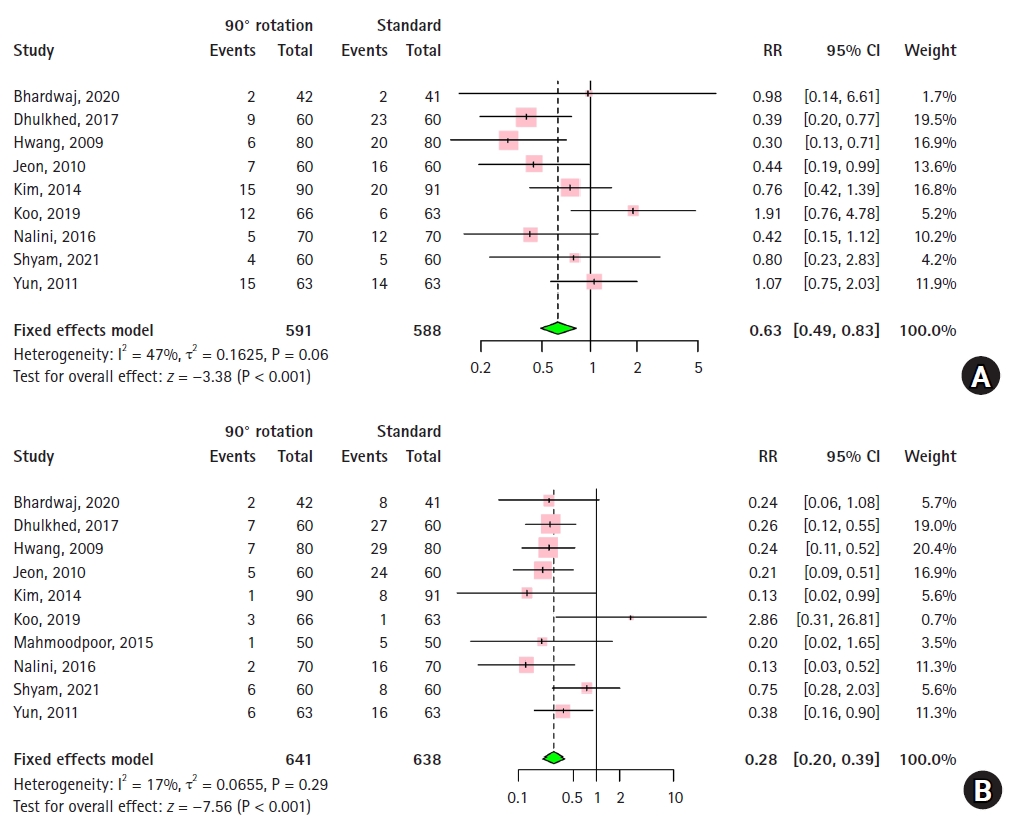
Table 1.
Characteristics of Included RCTs (n = 10)
| Author & Year | Sample size (standard/rotation) | Age | Type and size of SGA device | Cuff pressure | Allowance of manipulation | Type and doses of NMBA |
|---|---|---|---|---|---|---|
| Bhardwaj, 2020 [21] | 45/45 | 34.9 ± 10.9 | i-gelTM (3/4/5) | No cuff | Yes | Vecuronium 0.1 mg/kg |
| Dhulkhed, 2017 [22] | 60/60 | 28.8 ± 9.6 | ProsealTM (3/4) | Inflated | No | No |
| Hwang, 2009 [7] | 80/80 | 43.0 ± 11.1 | ProsealTM (3) | Deflated | Yes | No |
| Jeon, 2010 [8] | 60/60 | 49.0 ± 12.0 | ProsealTM (4/5) | Deflated | No | Rocuronium 0.6 mg/kg |
| Kim, 2014 [25] | 90/91 | 65.9 ± 9.9 | i-gelTM (3/4) | No cuff | Yes | Rocuronium 0.6 mg/kg |
| Koo, 2019 [13] | 66/63 | 44.8 ± 11.1 | FlexibleTM (3/4) | Deflated | Yes | Rocuronium 0.5 mg/kg |
| Mahmoodpoor, 2015 [23] | 50/50 | 62.5 ± 9.4 | ClassicTM | Inflated | No | No |
| Nalini, 2016 [24] | 70/70 | 38.9 ± 13.8 | ProsealTM (3/4) | Deflated | Yes | Atracurium 0.5 mg/kg |
| Shyam, 2021 [11] | 60/60 | 35.5 ± 12.0 | UniqueTM (3/4) | Deflated | Yes | Atracurium 0.05 mg/kg |
| Yun, 2011 [12] | 63/63 | 6.0 ± 2.0 | ProsealTM (2/2.5/3) | Deflated | No | Rocuronium 0.6 mg/kg |
References
1. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013; 118: 251-70.


2. Simon LV, Torp KD. Laryngeal mask airway [Internet]. Treasure Island (FL): StatPearls publishing [updated 2022 Feb; cited 2021 Aug 5]. Available from www.ncbi.nlm.nih.gov/books/NBK482184
3. Nakayama S, Osaka Y, Yamashita M. The rotational technique with a partially inflated laryngeal mask airway improves the ease of insertion in children. Paediatr Anaesth 2002; 12: 416-9.


4. Kumar D, Khan M, Ishaq M. Rotational vs. standard smooth laryngeal mask airway insertion in adults. J Coll Physicians Surg Pak 2012; 22: 275-9. Erratum in: J Coll Physicians Surg Pak 2012; 22: 411.

5. Matta BF, Marsh DS, Nevin M. Laryngeal mask airway: a more successful method of insertion. J Clin Anesth 1995; 7: 132-5.


6. Wakeling HG, Butler PJ, Baxter PJ. The laryngeal mask airway: a comparison between two insertion techniques. Anesth Analg 1997; 85: 687-90.

7. Hwang JW, Park HP, Lim YJ, Do SH, Lee SC, Jeon YT. Comparison of two insertion techniques of ProSeal laryngeal mask airway: standard versus 90-degree rotation. Anesthesiology 2009; 110: 905-7.


8. Jeon YT, Na HS, Park SH, Oh AY, Park HP, Yun MJ, et al. Insertion of the ProSeal laryngeal mask airway is more successful with the 90 degrees rotation technique. Can J Anaesth 2010; 57: 211-5.


9. Kim DH, Chae YJ, Min SK, Ha EJ, Yoo JY. Lightwand-guided insertion of flexible reinforced laryngeal mask airway: comparison with standard digital manipulation insertion. Med Sci Monit 2021; 27: e928538.



10. Park JY, Yu J, Hong JH, Hwang JH, Kim YK. Head elevation and laryngeal mask airway Supreme insertion: a randomized controlled trial. Acta Anaesthesiol Scand 2021; 65: 343-50.


11. Shyam T, Selvaraj V. Airway management using LMA-evaluation of three insertional techniques-a prospective randomised study. J Anaesthesiol Clin Pharmacol 2021; 37: 108-13.



12. Yun MJ, Hwang JW, Park SH, Han SH, Park HP, Kim JH, et al. The 90° rotation technique improves the ease of insertion of the ProSeal™ laryngeal mask airway in children. Can J Anaesth 2011; 58: 379-83.


13. Koo BW, Oh AY, Hwang JW, Na HS, Min SW. Comparison of standard versus 90° rotation technique for LMA Flexible™ insertion: a randomized controlled trial. BMC Anesthesiol 2019; 19: 95.



14. Moher D, Liberati A, Tetzlaff J, Altman DG; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097.



15. Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898.

16. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ 2004; 328: 1490.



17. Higgins JP, Deeks JJ. Selecting studies and collecting data. In: Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 [Internet]. London: The Cochrane Collaboration [updated 2011 Mar; cited 2021 Nov 25]. Available from www.handbook.cochrane.org
18. Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 2019; 22: 153-60.



19. R core Team. A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria [Internet]. [updated 2020 Aug; cited 2021 Oct 1]. Available from https://www.R-project.org
20. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Soft 2010; 36: 1-48.

21. Bhardwaj M, Singhal SK, Rashmi , Dahiya A. A prospective randomised trial to compare three insertion techniques for i-gel™ placement: standard, reverse, and rotation. Indian J Anaesth 2020; 64: 618-23.



22. Dhulkhed PV, Khyadi SV, Jamale PB, Dhulkhed VK. A prospective randomised clinical trial for the comparison of two techniques for the insertion of proseal laryngeal mask airway in adults-index finger insertion technique versus 90° rotation technique. Turk J Anaesthesiol Reanim 2017; 45: 98-102.



23. Mahmoodpoor A, Golzari SE, Hamidi M, Hamidi M, Parish M, Soleimanpour H, et al. Comparison of three methods for laryngeal mask airway insertion in adults: standard, lateral and rotational. J Clin Anal Med 2015; 6: 53-6.

24. Nalini KB, Shivakumar S, Archana S, Sandhya Rani DC, Mohan CV. Comparison of three insertion techniques of ProSeal laryngeal mask airway: a randomized clinical trial. J Anaesthesiol Clin Pharmacol 2016; 32: 510-4.



25. Kim HC, Yoo DH, Kim HJ, Jeon YT, Hwang JW, Park HP. A prospective randomised comparison of two insertion methods for i-gel placement in anaesthetised paralysed patients: standard vs. rotational technique. Anaesthesia 2014; 69: 729-34.


26. Park JH, Lee JS, Nam SB, Ju JW, Kim MS. Standard versus rotation technique for insertion of supraglottic airway devices: systematic review and meta-analysis. Yonsei Med J 2016; 57: 987-97.



27. Brimacombe J, Keller C. The ProSeal laryngeal mask airway: a randomized, crossover study with the standard laryngeal mask airway in paralyzed, anesthetized patients. Anesthesiology 2000; 93: 104-9.










