Efficacy of ultrasound-guided transversalis fascia plane block in pediatric ureteroneocystostomy surgery
Article information
Ureteroneocystostomy is one of the primary methods to treat vesicoureteral reflux (VUR) in children. Although less invasive methods, such as laparoscopic or robotic surgery, have been developed, open surgeries are still commonly performed. Various medical treatments and regional anesthesia techniques have been used to treat post-surgical pain in children. The transversalis fascia is a structure that covers the inner plane of the abdominal muscles that includes the preperitoneal fat layer posteriorly. The transversalis fascia plane (TFP) block, which was first defined in 2009 to provide local anesthesia to this region, has been used to effectively manage pain in lower abdominal surgery [1,2]. The TFP block procedure, defined by Hebbard, aims to block the iliohypogastric and ilioinguinal nerves, which are the proximal branches of the T12 and L1 spinal nerves that run between the transversus abdominis muscle and the transversalis fascia [1]. The Face, Legs, Activity, Cry, Consolability (FLACC) scale is an observational pain rating method that was developed by Merkel et al. [3] in 1997 that is used to evaluate pain in children aged two months to seven years.
We present the efficacy of the TFP block in five pediatric patients who underwent bilateral or unilateral ureteroneocystostomy surgery. Written informed consent from the patients and their parents was obtained to both administer the block and publish the report.
Five pediatric patients aged 4–7 years without any history of other systemic diseases were admitted to the operating room for open ureteroneocystostomy surgery. General anesthesia induction was performed with 2 mg/kg propofol, 2 μg/kg fentanyl, and 0.6 mg/kg rocuronium, and the patients were intubated. Anesthesia was maintained with 1−2% sevoflurane, 50% O2, and 0.125–0.25 µg/kg/min remifentanil. A TFP block was planned preoperatively to provide perioperative and postoperative analgesia to the patient. While the patient was in the supine position, the operation area and the linear ultrasound (US) probe were prepared under sterile conditions. The US probe was placed on the anterior abdominal wall in the transverse plane, and the oblique externus, oblique internus, and trasversus abdominis muscles were visualized. The US probe was then directed laterally, and the fascia transversalis and preperitoneal adipose tissue were visualized. Using the in-plane technique, a 50 mm block needle was passed through the posterior tail of the transversus abdominis muscle, and the fascia transversalis plane was entered. After confirming needle placement using saline, 0.5 ml/kg of 0.25% bupivacaine was injected. The same procedure was repeated on the opposite side for patients with bilateral VUR. Paracetamol (10 mg/kg) was administered intravenously to all patients 30 min before the end of the operation and was repeated every 6 h for 24 h. Postoperatively, 0.06 mg/kg neostigmine and 0.03 mg/kg atropine were administered to antagonize the muscle relaxant effect, and the patients were awakened. Pain assessments were conducted using the FLACC scale at 1, 2, 4, 12, and 24 h post-operation. Oral ibuprofen (10 mg/kg) was available as a rescue analgesia for patients with a FLACC score ≥ 4.
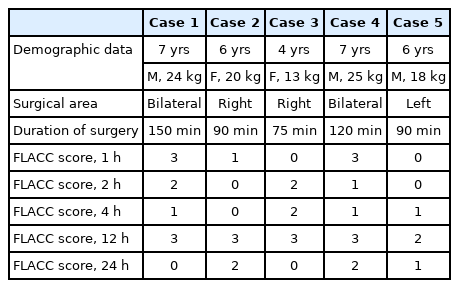
The patients’ demographic data and postoperative pain scores are presented in Table 1. None of the patients had a FLACC score ≥ 4 in the first 24 h postoperatively, and therefore no additional analgesics were necessary.
Currently, there are limited medical treatments available for managing postoperative pain in children undergoing ureteroneocystostomy surgery, particularly since the use of opioids is restricted in children [4]. Additionally, the use of non-steroidal anti-inflammatory drugs increases the risk of potential renal damage in this patient group. This highlights the importance of using regional anesthesia techniques to provide postoperative analgesia for these children. Caudal analgesia is one available method that provides adequate postoperative analgesia. However, it is associated with risks, such as dural punture, drug administration to the subarachnoid space, constipation, and hypotension [4]. In addition, the patient must be in a lateral decubitus position for administration and the hiatus sacralis may close prematurely in some children.
The use of plane blocks to prevent postoperative pain in patients undergoing ureteroneocystostomy surgery is currently uncommon, with very few studies particularly regarding pediatric patients undergoing ureteroneocystostomy. One previous report of a single pediatric case found that administering a TFP block effectively reduced postoperative pain after ureteroneocystostomy surgery [2]. The TFP block is a regional anesthesia technique that has been found to provide effective analgesia in the postoperative period after other lower abdominal surgeries. Specifically, it has been successfully used as intraoperative or postoperative analgesia for cesarean sections, inguinal hernias, and iliac crest grafts [5]. Efficacy may be increased in this population since the surgical procedures are located at the iliohypogastric nerve and ilioinguinal nerve dermatome areas. Compared to a caudal block, this regional anesthesia technique is less invasive and it is ergonomically easier to apply while the patient is in the supine position.
The FLACC scale includes five behaviors children exhibit in response to pain, which are graded from 0 to 2 points. The total score ranges from 0 to 10 points and is interpreted as follows: 0 points, comfortable; 1–3 points, mild pain; 4–6 points, moderate pain; 7–10 points, severe pain. None of the patients’ pain scores increased above four during follow-up in this case series, and therefore, no additional analgesic agents were necessary. These results indicate that TFP blocks may significantly reduce early postoperative pain in children who undergo ureteroneocystostomy surgery.
In conclusion, administering a TFP block before surgery provides effective postoperative analgesia in pediatric patients undergoing ureteroneocystostomy. However, an extensive series of randomized controlled studies is needed to confirm the efficacy and safety of this method in this patient population.
Notes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Uğur Peksöz (Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing)
Ahmet Murat Yayık (Funding acquisition; Investigation; Methodology; Resources; Software; Validation; Writing – original draft; Writing – review & editing)
Erkan Cem Çelik (Investigation; Methodology; Supervision; Visualization)