|
 |
| Korean J Anesthesiol > Volume 74(4); 2021 > Article |
|
Abstract
Background
Intravenous (IV) dexamethasone prolongs the duration of a peripheral nerve block; however, there is little available information about its optimal effective dose. This study aimed to evaluate the effects of three different doses of IV dexamethasone on the duration of postoperative analgesia to determine the optimal effective dose for a sciatic nerve block.
Methods
Patients scheduled for foot and ankle surgery were randomly assigned to receive normal saline or IV dexamethasone (2.5 mg, 5 mg, or 10 mg). An ultrasound-guided popliteal sciatic nerve block was performed using 0.75% ropivacaine (20 ml) before general anesthesia. The duration of postoperative analgesia was the primary outcome, and pain scores, use of rescue analgesia, onset time, adverse effects, and patient satisfaction were assessed as secondary outcomes.
Results
Compared with the control group, the postoperative analgesic duration of the sciatic nerve block was prolonged in groups receiving IV dexamethasone 10 mg (P < 0.001), but not in the groups receiving IV dexamethasone 2.5 mg or 5 mg. The use of rescue analgesics was significantly different among the four groups 24 h postoperatively (P = 0.001) and similar thereafter. However, pain scores were not significantly different among the four groups 24 h postoperatively. There were no statistically significant differences in the other secondary outcomes among the four groups.
Despite its efficacy, the main disadvantage of a single-injection peripheral nerve block is the limited duration of analgesia. To overcome this shortcoming, several adjuvants for local anesthetics (LAs) have been investigated [1ŌĆō4]. Among them, dexamethasone is an effective adjuvant, regardless of whether it is administered perineurally or intravenously [1]. However, perineural administration of dexamethasone remains an off-label use on account of its potential neurotoxicity [5]. In addition, there is concern about the potential hazard of precipitation when LA is mixed with dexamethasone [6]. Thus, intravenous (IV) administration of dexamethasone can be an alternative option, although perineural dexamethasone is superior to IV dexamethasone in prolonging postoperative analgesia as seen in a previous study [7]. In contrast to perineural dexamethasone, dose-finding studies investigating IV dexamethasone, especially for lower extremity blocks, remain scarce.
Therefore, we compared the effect of three different IV dexamethasone doses on postoperative analgesic duration after an ultrasound-guided popliteal sciatic nerve block to determine the optimal effective dose of dexamethasone as an adjuvant. We hypothesized that 2.5 mg, 5 mg, and 10 mg of IV dexamethasone would increase the postoperative analgesic duration of sciatic nerve block by at least 25% when compared with the control group.
This trial was approved by the Institutional Review Board of Inha University Hospital (Incheon, South Korea; #2016-050-014) and registered with the Clinical Trial Registry of Korea (https://cris.nih.go.kr/cris/index.jsp; identifier: KCT0002486; principal investigator: Jang Ho Song; date of registration: 04.04.2017) before patient enrollment. This prospective randomized study was undertaken at Inha University Hospital in accordance with the Helsinki Declaration. Adult inpatients with an American Society of Anesthesiologists physical status classification IŌĆōIII scheduled to undergo foot and ankle surgery, with surgical incision expected to be outside of the saphenous nerve territory, were enrolled between April 2017 and December 2018. In case of ankle fracture, we excluded patients who were expected to undergo surgical procedures with medial ankle incision and open reduction and internal fixation with plate fixation. Patients with contraindications to regional anesthesia, body mass index > 35 kg/m2, pre-existing neuropathy, diabetes, chronic steroid or opioid use, allergy to study medications, or pregnancy were also excluded. Written informed consent was obtained from all the patients.
Using a computer-generated random assignment and concealment method with sealed envelopes, patients were randomly allocated to receive IV saline 0.9% (control [group C]) or a dexamethasone (5 mg/ml) dose of 2.5 mg (group D2.5), 5 mg (group D5), or 10 mg (group D10) [8]. Sciatic nerve block was performed under ultrasound guidance using 20 ml of ropivacaine 0.75%. We chose ropivacaine to hasten the onset time of the block and prolong its duration [9ŌĆō11]. Sealed envelopes with the study group allocation were opened before the block placement, and study solutions were prepared with syringes containing 2 ml by one of the authors who was not involved in performing the blocks, patient care, or outcome assessment. The study drug was administered before the block placement. The anesthesiologist performing the blocks, surgeons, and outcome assessors were blinded to the group allocation.
Standard monitoring techniques, including electrocardiography, noninvasive blood pressure monitoring, and pulse oximetry, were applied to all patients along with supplemental oxygen on arrival to the induction room and used throughout the procedure. All patients were administered IV midazolam (0.03 mg/kg) and fentanyl (1 ┬Ąg/kg) for sedation and anxiolysis before the block. All the blocks were performed by the same anesthesiologist. Patients received the sciatic nerve block via a popliteal approach, with a portable ultrasound unit equipped with a 6ŌĆō13 MHz linear probe (Vivid q, GE Healthcare, USA) and an 80 mm 22-gauge needle (UniPlex NanoLine, Pajunk, Germany). The nerve stimulator was set at 0.5 mA, 0.1 ms, and 1 Hz. Patients were placed in the lateral decubitus position, with the operative leg in a non-dependent position. The tibial nerve was first identified in popliteal crease. Subsequently, probe was moved proximally until it merges with the common peroneal nerve. After disinfection and skin infiltration with 2% lidocaine (2 ml), the needle was advanced using an out-of-plane technique until its tip was positioned between the tibial and peroneal nerves inside the paraneural sheath [12]. A small volume (<1 ml) of saline was initially injected to ensure that the needle tip was correctly positioned. After the negative aspiration, 20 ml of ropivacaine 0.75% was injected incrementally. Any adverse events (such as vascular puncture, LA toxicity, or unintentional paresthesia) during the block administration were noted accordingly.
Following the LA administration, two investigators evaluated sensory and motor block onset every 5 min for 30 min. Sensory block was assessed in the tibial (plantar surface of the foot) and peroneal (dorsum of the foot) nerves using a cold test and as per the following scale: 0 = normal sensation; 1 = less cold; and 2 = not cold, when compared with the contralateral extremity. Motor block (plantar flexion of the tibial nerve and dorsiflexion of the peroneal nerve) was assessed using the following scale: 0 = no block; 1 = paresis; and 2 = paralysis. The onset times to sensory (time after completion of LA injection to loss of cold sensation in all nerve territories) and motor (time after completion of LA injection to paralysis of the tibial and peroneal nerve) blocks were recorded. Success of block was defined as analgesia in the tibial and peroneal nerves dermatomes and a lack of requirement for supplementary analgesia for pain in the surgical wound in the post-anesthesia care unit (PACU). Only patients with successful blocks were included in this study.
Due to the relatively long duration of tourniquet compression and assessment of the exact cause of postoperative pain (sciatic or saphenous nerve territory), patients underwent standard general anesthesia by a blinded attending anesthesiologist after the 30 min evaluation. Anesthesia was induced using propofol with endotracheal intubation facilitated by cisatracurium. Anesthesia was maintained using 40% oxygen in air mixture and 2ŌĆō3% sevoflurane. Muscle relaxation was antagonized using pyridostigmine and glycopyrrolate. After the surgical procedure, patients were transferred to the PACU and they stayed there until they met the PACU discharge criteria.
In the PACU, pain scores were assessed using a numerical rating scale (NRS) for pain (0 = no pain; 10 = worst possible pain) at 30 min after PACU arrival. Patients reporting an NRS score > 3 were administered IV fentanyl 25 ┬Ąg every 10 min until they were comfortable. Patients who reported medial ankle pain were excluded from the study.
Standardization of postoperative analgesia was carried out. All patients received 1 g of IV paracetamol every 6 h, irrespective of pain status. For rescue analgesia, patients were instructed to request analgesics (diclofenac 75 mg via intramuscular route) when an NRS of > 3 was reported on the operated foot or ankle. Persistent pain was treated with 50 mg IV tramadol. Further, meperidine 25 mg IV was administered to the patient in case of persistent pain, despite the use of diclofenac and tramadol.
The primary outcome was the duration of postoperative analgesia, which was defined as the time between the end of the LA injection and the first request for rescue analgesia for surgical pain in the operative extremity. For data analysis, patients who did not request any analgesics within the first 36 h had their duration of analgesia recorded as 36 h. The primary outcome was determined from their medical records. Secondary outcomes included pain scores, use of rescue analgesia, onset time to sensory and motor block, incidence of PONV, adverse effects, and patient satisfaction, respectively. An investigator blinded to group allocation assessed the following parameters 24 h after surgery: pain scores, incidence of PONV, adverse event(s), and patient satisfaction. The use of supplemental analgesics during the first 36 h after surgery was also recorded. The incidence of PONV was noted during the first 24 h after surgery. Any adverse events (e.g., paresthesia, numbness, or motor weakness) were also noted. Patient satisfaction was evaluated using an NRS (0 = very dissatisfied; 10 = very satisfied) [13]. Each patient was followed up with an attendant surgeon for 8 weeks to identify any neurological deficits or wound infection in the operative limb.
Sample size calculation was performed using data from a previous study that reported a postoperative analgesic duration of 15.4 h following a sciatic nerve block [14]. In the present study, a 4 h difference was considered clinically relevant. Assuming a standard deviation of 4 h, a calculated sample size of 18 patients was required for each group with a type I error of 0.05 and a power of 0.80. To allow for block failure and possible dropouts, 25 patients were included in each group.
Data are summarized as mean (standard deviation [SD]), median (Q1, Q3), or number (proportion [%]), as appropriate. Continuous variables were assessed for normality using the Kolmogorov-Smirnov test. The primary outcome was analyzed using the Kruskal-Wallis test, and differences between groups were analyzed using the Mann-Whitney U test with Bonferroni correction for multiple comparisons. The log-rank test was used to analyze the Kaplan-Meier plots for the block duration. Secondary outcomes were analyzed using the Kruskal-Wallis test or Pearson Žć2 test (or FisherŌĆÖs exact test) when appropriate. Differences were considered statistically significant at P < 0.05. For Bonferroni correction of multiple comparisons, P < 0.008 (0.05/6) was considered statistically significant. SPSS version 19.0 (IBM Corp., USA) for Windows (Microsoft Corp., USA) was used for statistical analysis.
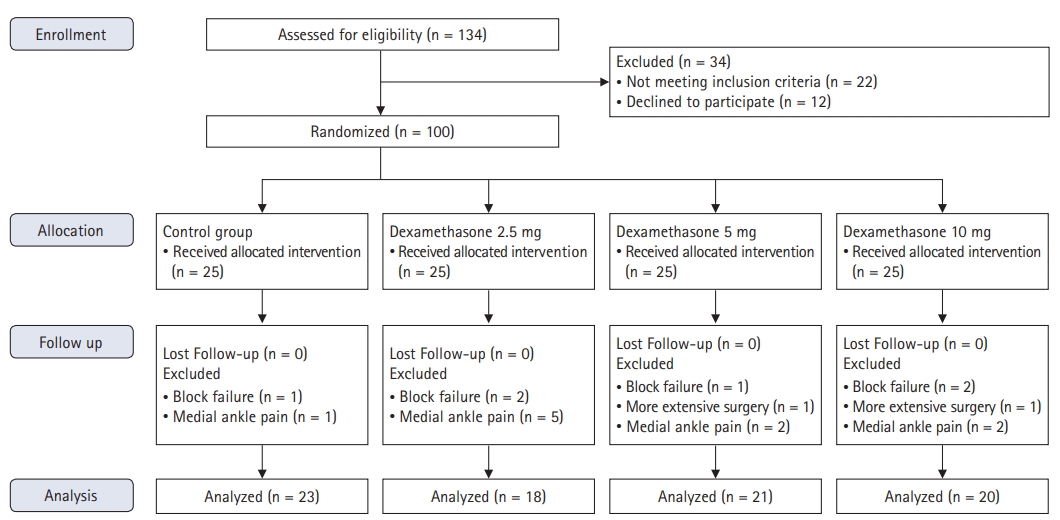
A total of 100 patients were recruited in this study. Eight patients were excluded after randomization due to block failure (n = 6) and/or unanticipated extensive surgery (two patients receiving autologous iliac crest bone grafting). Ten patients (one in group C, five in group D2.5, and two in groups D5 and D10) reported medial ankle pain and were hence excluded. The patient flow throughout the study is illustrated in Fig. 1. There were no significant differences among the four groups in terms of demographic or surgical data (Table 1). No significant differences in the onset time to sensory (P = 0.710) and motor block (P = 0.848) were observed among the four groups (Table 2). No adverse events during the block performance were observed in any of the groups.
The median duration of analgesia was as follows: group CŌĆö20.0 h (18.0ŌĆō25.5 h); group D2.5ŌĆö24.5 h (18.4ŌĆō27.8 h); group D5ŌĆö25.4 h (22.0ŌĆō31.5 h); and group D10ŌĆö29.1 h (25.7ŌĆō36.0 h). There were significant differences among the groups (Kruskal-Wallis chi-squared = 17.392; df = 3; P < 0.001). Compared with group C, the postoperative analgesic duration of sciatic nerve block was prolonged in group D10 (P < 0.001), but not in group D2.5 (P = 1.000) or D5 (P = 0.106). The Kaplan-Meier survival analysis of the primary outcome also suggested prolongation of analgesic duration in group D10 compared to group C and no detectable difference between groups D2.5 and D5 and group C (Fig. 2). For comparison of the survival distributions between the four groups, the log-rank chi-squared statistic was 13.2, with df = 3 (P = 0.004).
Differences in pain scores in the PACU and 24 h after surgery were not statistically significant among the groups (Table 2). In addition, there were no significant differences in the worst possible pain scores. However, there was a significant difference in the number of patients who requested rescue analgesics among the 4 groups at 24 h (Deviance = 15.85; df = 3; P = 0.001, Table 2), but not 24ŌĆō36 h after surgery. There were three, four, four, and seven patients in groups C, D2.5, D5, and D10, respectively, who did not request any rescue analgesics during the first 36 h after the block placement.
The four groups demonstrated a similar incidence of PONV (P = 0.723). In addition, no significant differences in adverse effects were observed among the four groups. Patient satisfaction was similar in all groups (P = 0.476) (Table 3). No neurological deficits or wound infections were observed in the patients on a follow-up visit performed by the surgeon 2ŌĆō4 weeks postoperatively.
We evaluated the effects of three different doses of IV dexamethasone on the postoperative analgesic duration of the sciatic nerve block. When compared with the control, only 10 mg of IV dexamethasone increased the duration of postoperative analgesia in the sciatic nerve block. Although the use of rescue analgesics was statistically different among the four groups 24 h after surgery, other secondary outcomes were similar among all the groups.
In this study, we observed a prolonged duration of sciatic nerve block following IV dexamethasone (10 mg). Although the precise mechanism was not clearly elucidated, this might be associated with the systemic anti-inflammatory effects of dexamethasone [15]. Several doses of dexamethasone have been used to prolong the duration of postoperative pain management. In the case of the perineural route, doses between 1 mg and 4 mg can increase the block duration in a dose-dependent manner [16]. A recent meta-analysis reported that 4 mg of perineural dexamethasone had a ceiling effect [17].
There were tendency of prolonged postoperative analgesia with increasing dosage of IV dexamethasone in the present study. However, only 10 mg of IV dexamethasone resulted in a statistically significant prolongation of postoperative analgesia for a sciatic nerve block. A previous study compared three different doses of IV dexamethasone with saline for an interscalene block [8]. The authors reported that IV dexamethasone 2.5 mg and 10 mg increased the duration of interscalene analgesia after shoulder surgery. The discrepancy between previous and current study may be described by the differences in the type of surgery. In contrast to upper extremity surgery, foot and ankle surgery require both saphenous and sciatic nerve blocks for complete anesthesia and analgesia. In this study, we did not perform a saphenous block in all patients. This incomplete block may have resulted that only the large amount of dose of IV dexamethasone prolonged the block duration. The saphenous nerve block as a supplement to a sciatic nerve block reduced the pain score after major ankle surgery [18]. In accordance with this study, we observed medial ankle pain in 10 patients, with 40% of arthrodesis and 60% of ankle fractures. However, another study reported that a continuous sciatic nerve block without saphenous nerve block provided adequate pain relief after moderately painful ankle and foot surgery [13], which was similar to the findings of this study. This suggested that the saphenous nerve was not a major factor for postoperative pain after moderately painful ankle and foot surgery. Another factor was the inadequate sample size of our study, which may have caused a type II error in the lower dose groups, even though it looks there were tendency of prolonged postoperative analgesia with increasing dosage of IV dexamethasone. Other factors may include differences in the type of nerve block, LA, or block technique, and the use of other postoperative analgesic modalities.
IV dexamethasone reduced inflammation and decreased postoperative pain and analgesic consumption [19,20]. Our study did not demonstrate a reduction of the worst and average pain scores in the dexamethasone group when compared with the control group. It was probably due to the infrequent assessment of pain score and the use of multimodal analgesia. Even though we did not assess cumulative opioid use, we could observe the number of patients who requested analgesics was different among the four groups at 24 h, but not at 24ŌĆō36 h after surgery. These findings suggest that IV dexamethasone did not reduce pain intensity, but delayed only the onset of pain after surgery.
In this study, we observed that approximately 30ŌĆō40% of the patients had residual motor weakness after 24 h. Previous studies have reported that IV dexamethasone results in prolonged motor block as well as sensory block [21ŌĆō23]. Prolonged motor weakness might be an undesirable block-related side effect since it might delay early mobilization and decrease patient satisfaction [9]. Thus, a lower concentration of LA may be a better choice to minimize this side effect.
Dexamethasone has been widely used as an effective prophylaxis for PONV [24]; however, in this study, there were no significant differences in the incidence of PONV. In addition, no differences were found among the four groups in terms of adverse effects and wound healing. These findings may be related to the fact that our study was not powered to evaluate such a difference.
This study had several limitations. The primary limitation was that different types of foot and ankle surgeries were included in our study, each with different degrees of expected postoperative pain. Second, we included surgeries that involved territories which is innervated mainly by the sciatic nerve. Especially the distal tibia and medial ankle joint, however, are innervated by the saphenous nerve [25], it is necessary to block both nerves for complete postoperative analgesia. This may have hence weakened our findings. Third, the primary outcome was the time to the first analgesic request. Since systemic dexamethasone can affect pain scores and opioid consumption [19,20], other outcome variables, such as duration of sensory or motor block, would have been more applicable in such cases. Fourth, all patients received general anesthesia, which could have affected the measured variables. Finally, 20 ml of 0.75% ropivacaine was used in this study. The main purpose of this study was to determine the dose-related effect of IV dexamethasone on the block duration following sciatic nerve block. For this reason, it is believed that the use of a lower concentration of ropivacaine for sciatic nerve block could make a bigger difference. In addition, our findings cannot be extrapolated to other concentrations and volumes of LA or other types of LA.
In conclusion, the results of the present study demonstrated that compared to the control group, only IV dexamethasone 10 mg increased the duration of postoperative analgesia following a sciatic nerve block for foot and ankle surgery without the occurrence of adverse events.
NOTES
Author Contributions
Byung-Gun Kim (Writing ŌĆō original draft)
Woojoo Lee (Formal analysis)
Jang Ho Song (Conceptualization; Methodology)
Chunwoo Yang (Conceptualization; Funding acquisition; Methodology; Writing ŌĆō original draft)
Gyung A Heo (Data curation; Investigation)
Hongseok Kim (Data curation)
Fig.┬Ā2.
Kaplan-Meier survival plot illustrating the duration of postoperative analgesia in the study groups. Group C: control group, Group D2.5: dexamethasone 2.5 mg, Group D5: dexamethasone 5 mg, Group D10: dexamethasone 10 mg. *P = 0.004 (log-rank test) compared to control group.

Table┬Ā1.
Demographic and Surgical Data
Table┬Ā2.
Secondary Outcomes of Onset Time to Sensory and Motor Block, Pain Scores, and Rescue Analgesics
| Outcome | Group C (n = 23) |
Dexamethasone |
P value | ||
|---|---|---|---|---|---|
| Group D2.5 (n = 18) | Group D5 (n = 21) | Group D10 (n = 20) | |||
| Onset time (min) | |||||
| ŌĆāSensory block | 10 (10, 15) | 15 (6, 25) | 15 (8, 20) | 15 (10, 15) | 0.710 |
| ŌĆāMotor block | 20 (15, 30) | 25 (11, 30) | 25 (20, 30) | 20 (15, 30) | 0.848 |
| Pain score | |||||
| ŌĆāIn PACU | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0.337 |
| ŌĆāAt 24 h | 3 (0, 5) | 5 (3, 6) | 4 (2, 5) | 3 (0, 5) | 0.147 |
| ŌĆāWorst possible pain | 7 (4, 8) | 8 (4, 9) | 6 (3, 9) | 4 (1, 8) | 0.139 |
| Rescue analgesics* | |||||
| ŌĆā0ŌĆō24 h after surgery | 20 (87)/7 (30) | 12 (67)/3 (17) | 11 (52)/5 (24) | 6 (30)/4 (20) | 0.001 |
| ŌĆā24ŌĆō36 h after surgery | 10 (43)/2 (9) | 6 (33)/0 (0) | 11 (52)/2 (10) | 9 (45)/0 (0) | 0.516 |
Values are presented as median (Q1, Q3) or number (%). *Rescue analgesics was presented as number of patients (%) using non-opioid/opioid analgesics. PACU: post-anesthesia care unit. Group C: control group, Group D2.5: dexamethasone 2.5 mg, Group D5: dexamethasone 5 mg, Group D10: dexamethasone 10 mg.
Table┬Ā3.
Secondary Outcomes of Incidence of PONV, Adverse Effects, and Patient Satisfaction
References
1. Kang R, Jeong JS, Yoo JC, Lee JH, Choi SJ, Gwak MS, et al. Effective dose of intravenous dexmedetomidine to prolong the analgesic duration of interscalene brachial plexus block: a single-center, prospective, double-blind, randomized controlled trial. Reg Anesth Pain Med 2018; 43: 488-95.

2. Desmet M, Braems H, Reynvoet M, Plasschaert S, Van Cauwelaert J, Pottel H, et al. I.V. and perineural dexamethasone are equivalent in increasing the analgesic duration of a single-shot interscalene block with ropivacaine for shoulder surgery: a prospective, randomized, placebo-controlled study. Br J Anaesth 2013; 111: 445-52.


3. Seervi SN, Singariya G, Kamal M, Kumari K, Siddeshwara A, Ujwal S. Effect of addition of buprenorphine or dexamethasone to levobupivacaine on postoperative analgesia in ultrasound guided transversus abdominis plane block in patients undergoing unilateral inguinal hernia repair: a prospective randomized double blind controlled trial. Korean J Anesthesiol 2019; 72: 245-52.



4. Adnan T, Elif AA, Ayse K, Gulnaz A. Clonidine as an adjuvant for lidocaine in axillary brachial plexus block in patients with chronic renal failure. Acta Anaesthesiol Scand 2005; 49: 563-8.


5. Williams BA, Hough KA, Tsui BY, Ibinson JW, Gold MS, Gebhart GF. Neurotoxicity of adjuvants used in perineural anesthesia and analgesia in comparison with ropivacaine. Reg Anesth Pain Med 2011; 36: 225-30.



6. Hwang H, Park J, Lee WK, Lee WH, Leigh JH, Lee JJ, et al. Crystallization of local anesthetics when mixed with corticosteroid solutions. Ann Rehabil Med 2016; 40: 21-7.



7. Baeriswyl M, Kirkham KR, Jacot-Guillarmod A, Albrecht E. Efficacy of perineural vs systemic dexamethasone to prolong analgesia after peripheral nerve block: a systematic review and meta-analysis. Br J Anaesth 2017; 119: 183-91.


8. Desmet M, Vanneste B, Reynvoet M, Van Cauwelaert J, Verhelst L, Pottel H, et al. A randomised controlled trial of intravenous dexamethasone combined with interscalene brachial plexus blockade for shoulder surgery. Anaesthesia 2015; 70: 1180-5.


9. Fredrickson MJ, Smith KR, Wong AC. Importance of volume and concentration for ropivacaine interscalene block in preventing recovery room pain and minimizing motor block after shoulder surgery. Anesthesiology 2010; 112: 1374-81.


10. Fenten MG, Schoenmakers KP, Heesterbeek PJ, Scheffer GJ, Stienstra R. Effect of local anesthetic concentration, dose and volume on the duration of single-injection ultrasound-guided axillary brachial plexus block with mepivacaine: a randomized controlled trial. BMC Anesthesiol 2015; 15: 130.



11. Casati A, Fanelli G, Borghi B, Torri G. Ropivacaine or 2% mepivacaine for lower limb peripheral nerve blocks. Study Group on Orthopedic Anesthesia of the Italian Society of Anesthesia, Analgesia, and Intensive Care. Anesthesiology 1999; 90: 1047-52.


12. Techasuk W, Bernucci F, Cupido T, Gonzalez AP, Correa JA, Finlayson RJ, et al. Minimum effective volume of combined lidocaine-bupivacaine for analgesic subparaneural popliteal sciatic nerve block. Reg Anesth Pain Med 2014; 39: 108-11.


13. Ilfeld BM, Morey TE, Wang RD, Enneking FK. Continuous popliteal sciatic nerve block for postoperative pain control at home: a randomized, double-blinded, placebo-controlled study. Anesthesiology 2002; 97: 959-65.

14. Sinardi D, Marino A, Chillemi S, Siliotti R, Mondello E. Sciatic nerve block with lateral popliteal approach for hallux vagus correction. Comparison between 0.5% bupivacaine and 0.75% ropivacaine. Minerva Anestesiol 2004; 70: 625-9.

15. Yilmaz-Rastoder E, Gold MS, Hough KA, Gebhart GF, Williams BA. Effect of adjuvant drugs on the action of local anesthetics in isolated rat sciatic nerves. Reg Anesth Pain Med 2012; 37: 403-9.



16. Albrecht E, Reynvoet M, Fournier N, Desmet M. Dose-response relationship of perineural dexamethasone for interscalene brachial plexus block: a randomised, controlled, triple-blind trial. Anaesthesia 2019; 74: 1001-8.


17. Kirkham KR, Jacot-Guillarmod A, Albrecht E. Optimal dose of perineural dexamethasone to prolong analgesia after brachial plexus blockade: a systematic review and meta-analysis. Anesth Analg 2018; 126: 270-9.


18. Bj├Ėrn S, Wong WY, Baas J, Nielsen KK, B├Ėrglum J, Hauritz RW, et al. The importance of the saphenous nerve block for analgesia following major ankle surgery: a randomized, controlled, double-blind study. Reg Anesth Pain Med 2018; 43: 474-9.

19. Mattila K, Kontinen VK, Kalso E, Hynynen MJ. Dexamethasone decreases oxycodone consumption following osteotomy of the first metatarsal bone: a randomized controlled trial in day surgery. Acta Anaesthesiol Scand 2010; 54: 268-76.


20. De Oliveira GS Jr, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology 2011; 115: 575-88.
21. Sakae TM, Marchioro P, Schuelter-Trevisol F, Trevisol DJ. Dexamethasone as a ropivacaine adjuvant for ultrasound-guided interscalene brachial plexus block: a randomized, double-blinded clinical trial. J Clin Anesth 2017; 38: 133-6.


22. Abdallah FW, Johnson J, Chan V, Murgatroyd H, Ghafari M, Ami N, et al. Intravenous dexamethasone and perineural dexamethasone similarly prolong the duration of analgesia after supraclavicular brachial plexus block: a randomized, triple-arm, double-blind, placebo-controlled trial. Reg Anesth Pain Med 2015; 40: 125-32.

23. Dawson RL, McLeod DH, Koerber JP, Plummer JL, Dracopoulos GC. A randomised controlled trial of perineural vs intravenous dexamethasone for foot surgery. Anaesthesia 2016; 71: 285-90.