 |
 |
| Korean J Anesthesiol > Volume 74(4); 2021 > Article |
|
Rhomboid intercostal block (RIB) is a novel block that may be used for several indications such as thoracic procedures and myofascial pain [1,2]. It may be performed for open thoracotomy [3]; however, more information is needed for other thoracic procedures. Video-assisted thoracic surgery (VATS) has the advantage of reduced pain over open thoracotomy. However, patients may still experience moderate to severe pain after VATS [4]. Herein, we report the use of RIB in three patients for analgesia management after VATS. Written informed consent for the procedure and future publication was obtained from the patients.
Patient 1 was a 45-year-old male with 170 cm height and 75 kg weight. He was diagnosed with lung carcinoma of the right lung. He had no additional comorbidities and was American Society of Anesthesiologists physical status (ASA PS) classification I. Patient 2 was a 53-year-old male with 165 cm height and 72 kg weight. He was diagnosed with left lung carcinoma, had no additional comorbidities, and was ASA PS classification I. Patient 3 was a 58-year-old male who was 178 cm tall and weighed 86 kg. He was diagnosed with right lung carcinoma, had no additional comorbidities, and was ASA PS classification I. All of three patientsŌĆÖ blood tests were within normal ranges and vital signs were stable. The patients underwent thoracoscopic surgery lasting 130, 125, and 110 minutes, respectively for the patient 1, 2, and 3 with no complications during the surgery. After RIB, the patients were extubated. After observing sufficient spontaneous respiration, they were transferred to the intensive care unit (ICU) for further monitoring. Intravenous (IV) ibuprofen (400 mg), dosed at every 8 hours postoperatively was administered for postoperative pain control. The visual analogue score (VAS) was evaluated at 1, 6, 12, and 24 hours.
For patient 1, the static and dynamic (on deep breathing) VAS scores were 0/1, 1/2, 0/2, and 1/1, respectively. The patient needed no additional analgesic drugs. After 24 hours, the patient was transferred to the thoracic surgery ward. After 36 hours, the chest drain was removed. On the 4th day after surgery, the patient was discharged. For patient 2, the static and dynamic VAS scores were 1/2, 2/3, 1/3, and 0/1, respectively. He needed no additional analgesic drugs. After 24 hours, he was transferred to the ward. After 48 hours, the chest drain was removed. On the 5th day after surgery, the patient was discharged. For patient 3, the static and dynamic VAS scores were 0/2, 1/2, 1/1, and 0/1, respectively. He needed no additional analgesic drugs. After 24 hours, he transferred to the ward. After 36 hours, the chest drain was removed. On the 3rd postoperative day, he was discharged.
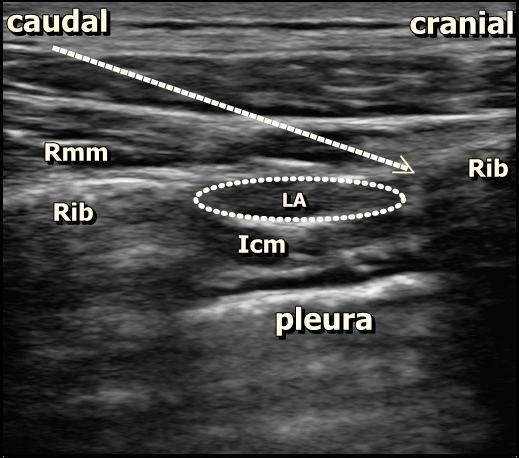
All patients underwent unilateral thoracoscopic lobectomy due to lung carcinoma. A standard three-port VATS approach (at the 5th, 8th, and 9th intercostal space) was performed. A 24 F chest tube was placed at 8th intercostal space in the midaxillary line. General anesthesia induction was performed using IV propofol (2 mg/kg), fentanyl (1.5 ┬Ąg/kg), and rocuronium bromide (0.6 mg/kg). A double-lumen tube was used for orotracheal intubation and its position was confirmed via fiberoptic bronchoscopy. The patients were placed in a lateral decubitus position for surgery. Mechanical ventilation was performed using a one-lung mechanical ventilation model. Perioperative analgesia was provided with a remifentanil infusion at a rate of 0.01ŌĆō0.1 ┬Ąg/kg/min. A dose of 400 mg ibuprofen and tramadol 100 mg was administered IV 20 minutes before the end of the surgery for multimodal postoperative pain management. At the end of the surgery, RIB was performed in the lateral decubitus position using a Vivid-q US system (GE Healthcare, USA) in these three patients. The same regional block technique was administered, and the same dosages of drugs were applied to the patients. After placing a linear high-frequency probe (12 MHz) medially in the sagittal plane on the medial border of the scapula at the T5-6 level, a 22 G, 80 mm needle (Braun Stimuplex Ultra, 360 30┬░) was inserted into the fascial plane between the rhomboid major and intercostal muscles in a caudal cranial direction. A dose of 20 ml 0.25% bupivacaine was injected into the fascial plane (Fig. 1).
As a new technique, the RIB defined by Elsharkawy et al. [5] in 2016 according to a cadaveric examination may be a good alternative for chest wall analgesia. This cadaveric examination of the RIB using methylene blue contrast dye showed the spread of dye from caudad to cephalad, including the T2-T8 tissue plane, as far as the lateral branches of the intercostal nerves T3-T8, the posterior primary rami near the midline, and the clavipectoral fascia within the axilla. The authors concluded that RIB may be effective for managing anterior and posterior hemithorax pain [5]. The analgesic efficacy of RIB after thoracotomy has been reported by Altiparmak et al. [3], who demonstrated that RIB provided good postoperative pain management in two patients for thoracotomy. In this paper, we also demonstrated that RIB provides effective analgesia for VATS in three patients.
In conclusion, RIB may be an alternative technique for pain management after VATS. There is a requirement for a larger comparative study to decide and advise regarding its practical applications in routine analgesic modality.
NOTES
Author Contributions
Bahad─▒r ├ćift├¦i (Conceptualization; Investigation; Methodology; Writing ŌĆō original draft; Writing ŌĆō review & editing)
Mursel Ekinci (Conceptualization; Investigation; Methodology; Writing ŌĆō original draft)
Yunus Oktay Atalay (Conceptualization; Data curation; Investigation; Methodology; Writing ŌĆō review & editing)
Fig.┬Ā1.
Sonographic anatomy of block, needle direction, and spread of local anesthetic (LA). The rhomboid major muscle (Rmm), intercostal muscle (Icm), and rib are seen. The white arrow indicates the direction of the needle.
References
1. Elsharkawy H, Hamadnalla H, Altinpulluk EY, Gabriel RA. Rhomboid intercostal and subserratus plane block -a case series. Korean J Anesthesiol 2020; 73: 550-6.

2. Ekinci M, Ciftci B, Alici HA, Ahiskalioglu A. Ultrasound-guided rhomboid intercostal block effectively manages myofascial pain. Korean J Anesthesiol 2020; 73: 564-5.

3. Alt─▒parmak B, Korkmaz Toker M, Uysal A─░, Turan M, G├╝m├╝┼¤ Demirbilek S. The usage of single-shot ultrasound guided rhomboid intercostal block for analgesia after thoracotomy: clinical experience in two patients. J Clin Anesth 2019; 56: 98-9.











