Introduction
Interscalene brachial plexus block (ISB) has been shown to provide excellent analgesia for shoulder surgery and has been the standard regional anesthesia technique used for decades. However, some studies have quoted up to 100% incidence of phrenic nerve palsy [
1]. This results in hemidiaphragmatic paresis and approximately 25ŌĆō30% reduction in pulmonary function [
2]. For patients with limited respiratory reserves, such as the morbidly obese [
3], patients with chronic obstructive lung disease (COPD) [
4], and the elderly, this reduction can result in symptomatic dyspnea or desaturation. While the opioid-sparing effects of regional anesthesia are most valuable to these groups of patients, they are least likely to tolerate the reduction in lung function caused by an ISB. In addition, ISB is also associated with other adverse effects such as HornerŌĆÖs syndrome, hoarseness of voice, and dense motor blockade.
Suprascapular nerve block (SSB) has been proposed as an alternative to the ISB in providing analgesia for shoulder surgeries as it has a lower likelihood of causing phrenic nerve blockade [
5]. The suprascapular nerve innervates approximately 60ŌĆō70% of the shoulder joint. There are two approaches to performing the SSB; posteriorly, in the supraspinous fossa, and anteriorly, in the supraclavicular fossa. There are concerns that local anesthetic deposited via the anterior approach may still spread to the phrenic nerve and result in some degree of impairment of lung function.
The primary aim of this study is to investigate the effect of ISB and SSB (anterior and posterior approaches) on pulmonary function, forced vital capacity (FVC), and forced expiratory volume in 1 second (FEV1). Our secondary aim is to compare their analgesic efficacy (pain scores and opioid consumption) and other adverse effects.
Materials and Methods
This study was approved by the Institutional Ethics Board (SingHealth CIRB, reference 2017/2459) and registered on clinicaltrials.gov, NCT03277326. Written, informed consent was obtained from 60 patients undergoing arthroscopic shoulder surgery.
Patients scheduled for elective arthroscopic shoulder surgery under general anesthesia, aged 21 years old and above, American Society of Anesthesiologist physical status classification 1 to 3 and body mass index 18ŌĆō35 kg/m2 were included in this study. We excluded patients who were unable to give consent, were on chronic opioid therapy, allergic to drugs used in the study, had pre-existing neurological deficits, had pre-existing lung disease (COPD, uncontrolled asthma), and had any contraindications for regional anesthesia such as coagulopathy.
The patients were randomly assigned to three groups using a computer-generated block randomization list with allocation concealment. The primary anesthesiologist and data collector were blinded. Due to the nature of the study, the investigator performing the block could not be blinded. Sham blocks were not performed for ethical reasons and to avoid risk of unnecessary harm to patients.
On the day of admission, prior to surgery, a baseline FVC and FEV1 were measured using a bedside spirometer (Vitalograph ALPHA
TM, USA) in a seated position. Patients were instructed on how to use the spirometer and average readings of three attempts were used for analysis. In addition, bilateral diaphragmatic excursion, in centimeters, was measured by ultrasound using the anterior subcostal view, below the subcostal margin in the mid-clavicular line [
6], during a vital capacity breath, using a 2ŌĆō5 Hz low frequency curvilinear probe (Sonosite Edge
TM, FUJIFILM Sonosite Inc., USA). Premedication of oral paracetamol 1 g was administered 30 min preoperatively. The block was performed by one of the study investigators, who are competent in all three block techniques. Intravenous access was obtained and sedation with midazolam (up to 3 mg) was administered as required. Standard monitors were applied and supplementary oxygen was provided during the block. ISB, anterior and posterior approaches to SSB were performed under real time ultrasound guidance, Sonosite Edge, USA. In each group, 15 ml of 0.5% ropivacaine (75 mg of ropivacaine) was used for the block.
The ISB and anterior SSB were performed with the patient in a supine position, with the head turned to the contralateral side. For ISB, an ultrasound scan was performed to identify the C5, C6, and C7 nerve roots between the scalene muscles (
Fig. 1). Local anesthetic was deposited between the C5 and C6 nerve roots, within the interscalene groove. For anterior SSB, the nerve was traced as it diverged from the brachial plexus to lie under the omohyoid muscle in the supraclavicular fossa [
7] (
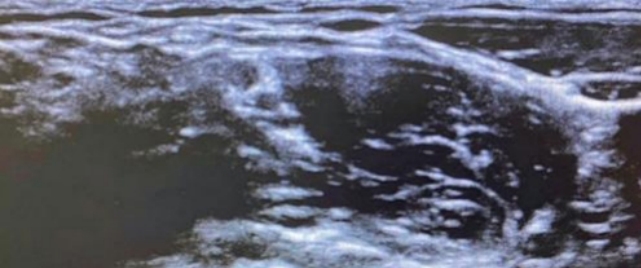
Fig. 2). Local anesthetic was deposited lateral to the suprascapular nerve, underneath the omohyoid muscle. Posterior SSB was performed with the patient in the seated position and the supraspinous fossa was identified by ultrasonography (
Fig. 3). Local anesthetic was deposited in the supraspinous fossa, beneath the superior transverse scapular ligament and supraspinatus muscle [
8].
Block success was assessed 30 min after performing the block by assessing the degree of sensory and motor blockade. Sensory block was tested by applying an ice block over the cutaneous innervation of the respective nerves: the deltoid area for the axillary nerve, back of scapular for the suprascapular nerve, the lateral palm for the median nerve, the lateral aspect of the forearm for the musculocutaneous nerve, the lateral aspect of the back of the hand for the radial nerve, and the little finger for the ulnar nerve. Motor innervation was tested by assessing the strength of these movements: arm abduction for the axillary nerve, internal rotation of the arm for the suprascapular nerve, thumb opposition for the median nerve, elbow flexion for the musculocutaneous, elbow extension for the radial nerve, and finger abduction for the ulna nerve. Pulmonary function tests as described earlier were repeated.
General anesthesia was induced with intravenous fentanyl (up to 2 ╬╝g/kg), propofol (1ŌĆō3 mg/kg), and atracurium (0.5 mg/kg). An endotracheal tube was used to maintain the airway and anesthesia was maintained on an oxygen/air/volatile agent mixture. Intravenous morphine (up to 0.2 mg/kg) was administered intraoperatively for analgesia, as required. The total amount of intraoperative opioids used was recorded. Intravenous ondansetron was given at the end of surgery for anti-emesis.
In the recovery area, intravenous morphine (up to 0.2 mg/kg) was administered to achieve a pain score of less than 3 before discharge to the ward. Regular oral paracetamol 1 g every 6 hours and etoricoxib 120 mg once daily was prescribed for postoperative analgesia. Oxycodone 5 mg every 6 hours, as required, was administered for breakthrough pain.
The primary endpoint was the degree of reduction from baseline pulmonary function after the block. Pain scores at rest and on movement were recorded at 1, 6, 12, and 24-hour periods, after surgery, using an 11-point numeric rating scale. Patients were assessed at 24 hours for total opioid (oxycodone) consumption and any adverse effects (postoperative nausea and vomiting, sedation, HornerŌĆÖs syndrome, and hoarseness of voice).
Statistical analysis
The sample size was based on the study by Auyong et al. [
9] where lung function (mean vital capacity) was reduced by 38% (SD 18) in the ISB group and 18% in the anterior suprascapular group. We aimed to detect a difference of Ōēź18% between groups in terms of reduction in lung function. For the study to have a power of 80% and a two-tailed P value of 0.05, we required at least 17 patients per group. We recruited 20 patients per group to account for possible cases of drop-out/loss to follow-up.
Data were analyzed using SPSS for Windows (SPSS ver. 20. IBM Inc., USA). Categorical data are presented as percentage and frequency. Parametric numerical data are presented as mean and standard deviation, while non-parametric data are presented as median (interquartile range). Categorical outcomes were analyzed with Chi-square test or FisherŌĆÖs exact test. Numerical data were compared among the groups with one-way ANOVA and non-parametric data with the KruskalŌĆōWallis test. Bonferroni correction was used to adjust for multiple comparisons. A two-tailed P value of < 0.05 was considered statistically significant.
Results
The study was conducted from September 2017 to April 2018 in Changi General Hospital, Singapore. Sixty-eight patients were assessed for eligibility to be recruited for the study, of which six patients were not eligible and two patients refused to participate. Finally, 60 patients provided written, informed consent to participate in this study and were randomized according to the study protocol. All patients received the intended intervention; follow-up was completed and data were analyzed. CONSORT diagram of patient recruitment is in
Fig. 4. The baseline demographics are presented in
Table 1. There were no statistically significant differences with respect to age, sex, and ASA classification.
Block success was assessed after 30 min; the results are presented in
Table 2. All three groups had high success rates of blocakade of the suprascapular nerve (90ŌĆō100%). The majority of patients who received ISB also showed blockade of other nerves in the brachial plexus, except the ulnar nerve, which was blocked in a small proportion of patients. Some patients who received SSB also showed blockade of the axillary nerve, especially with the anterior approach. Patients who received posterior SSB did not have any blockade of the median, ulnar, radial, and musculocutaneous nerves.
The respiratory effects of the different blocks are reported in
Table 3. There was a significant reduction in FVC, FEV1, and diaphragmatic excursion of the ipsilateral side in patients receiving ISB, compared to those receiving SSB. The ISB group had a reduction of FVC of mean ┬▒ SD, 31.2% ┬▒ 17.5% while the anterior and posterior SSB groups had significantly less reduction of FVC by 3.6% ┬▒ 18.6% and 6.8% ┬▒ 6.5%, respectively (P < 0.001). Similarly, the diaphragmatic excursion decreased more in the ISB group than in the anterior and posterior SSB groups (median [IQR]): -85. 7% (-95.3% to -63.3%) vs. -1.8% (-13.1% to 2.3%) and -1.2% (-8.8% to 16.8%), respectively (P < 0.001).
The analgesic effects of the different blocks are presented in
Table 4. Median pain scores (IQR) in ISB and anterior SSB groups were lower than those in the posterior SSB group at 6 hours on movement: 0 (0ŌĆō2), 1.8 (0ŌĆō4.5) vs. 5 (2.5ŌĆō8), respectively (P = 0.002). At 12 hours, pain scores on movement were also higher in the posterior SSB group than in the ISB group: ISB 2 (0ŌĆō5), anterior SSB 4 (2ŌĆō6.8) vs posterior SSB 6 (3ŌĆō7.5), respectively (P = 0.017).
There was no statistically significant difference in intraoperative opioid consumption between the groups. The posterior SSB group had a trend toward requiring increased levels of morphine in recovery but this was not statistically significant after BonferroniŌĆÖs correction. There was no statistically significant difference in 24-hour oxycodone consumption; 65% of patients in the ISB group required oxycodone in the first 24 hours compared to 45% in the anterior SSB group and 35% in the posterior SSB group.
There were no statistically significant differences in opioid-related side effects such as sedation, nausea, and vomiting. None of the 60 patients were sedated. None of the patients in the ISB group had nausea and vomiting while two patients in the anterior SSB group had nausea, out of which one had vomiting, and two in the posterior SSB group had nausea and vomiting.
Regarding complications, the ISB group had one patient with hoarseness of voice and one patient with HornerŌĆÖs syndrome. No patient complained of dyspnea or had desaturation. No patient had other block-related complications such as bleeding, hematoma, infection, or nerve injury.
Discussion
The results of our study showed that both approaches of SSB preserved lung function compared to the ISB, which resulted in a decrease in FVC, FEV1, and diaphragmatic excursion. The analgesic effect of the anterior SSB and ISB were superior to that provided by the posterior SSB. Two patients in the ISB group had adverse effects; one patient had HornerŌĆÖs syndrome and another patient experienced hoarseness of voice.
ISB is considered the gold standard for peri-operative analgesia for shoulder surgeries. However, as the phrenic nerve lies close to the interscalene groove, ISB is associated with phrenic nerve paresis in up to 100% of cases [
1], resulting in ipsilateral hemidiaphragmatic paresis. Though well tolerated in healthy patients, patients with decreased respiratory function may experience symptomatic dyspnea or hypoxia. Various methods to avoid this adverse effect, including low-volume [
10] and extra-fascial injections [
11], have been attempted with limited success. Blockade of the suprascapular nerve, alone or in combination with the axillary nerve, have been suggested as an alternative means of analgesia, which could minimize the risk of phrenic nerve paresis [
12,
13].
The SSB was first described by Wertheim and Rovenstein [
14] in 1941 for chronic shoulder pain and performed in the suprascapular fossa. The ultrasound-guided SSB technique was subsequently described by Harmon and Hearty in 2007 [
8]. In this study, we had referred to this technique as the posterior SSB. However, several studies had shown that the analgesic effects were inferior to those of an ISB [
12,
13,
15]. Siegenthaler et al. [
7] described a new technique of blocking the suprascapular nerve in the supraclavicular fossa, and we used this as the anterior SSB in our study.
There is a paucity of studies on SSB using the anterior approach. Auyong et al. [
9] investigated the effect on lung function from continuous ISB, supraclavicular, and anterior SSB and found less reduction of lung function with the anterior SSB (18%) than with ISB (38%). Weigel et al. [
16] compared ISB with anterior SSB and showed that pain scores with SSB were not inferior to those with ISB. However, their study did not investigate the effect on lung function.
As posterior SSB is performed well away from the phrenic nerve, one would expect no reduction in lung function. Some studies have shown that supraclavicular brachial plexus block results in impairment of respiratory function, possibly due to retrograde spread of local anesthetics [
17]. This could suggest that anterior SSB performed in the supraclavicular fossa may have similar effects on respiratory function.
On the contrary, we demonstrated that lung function (FVC and FEV1) was preserved in both the anterior and posterior SSB groups compared to in the ISB group, which showed a reduction in lung function by almost a third from the baseline. Similarly, ipsilateral diaphragmatic excursion was preserved in patients who received a suprascapular block but drastically reduced in the ISB group. A recent study by Ferre et al. [
18] showed an incidence of hemidiaphragmatic paralysis of 40% in the anterior SSB group and 2% in the posterior SSB group. A possible explanation could be that in our study, we intentionally scanned as distally as possible to isolate the suprascapular nerve and inject the agent lateral to the nerve to minimize deposition of the local anesthetic near the rest of the brachial plexus or the phrenic nerve.
FVC and FEV1 were chosen as parameters easily reproducible using a bedside spirometer. Studies have shown that FEV1 is strongly and positively correlated with diaphragmatic function [
19,
20]. UrmeyŌĆÖs study demonstrated a reduction of FVC by 27% ┬▒ 4.3% and FEV1 of 26.4% ┬▒ 6.8% after ISB; our results were similar [
2].
We chose to use 15 ml of 0.5% ropivacaine as this was the standard volume used for a single-shot brachial plexus block in our institution. Although a small volume could have been used to achieve intraoperative analgesia, the effects of the block may wear off rapidly. Despite the volume used in this study, there was little evidence of retrograde spread of local anesthetic from the anterior SSB to the phrenic nerve and minimal effect on the other major nerves of the brachial plexus.
Concerning analgesic efficacy, we found no statistically significant differences in pain scores at 6, 12, and 24 hours postoperatively between the anterior SSB and ISB groups. Our results are congruent with those of AuyongŌĆÖs recent study [
21] comparing single-shot anterior SSB, supraclavicular, and interscalene blocks, which showed that anterior SSB provided non-inferior analgesia than interscalene and also preserved vital capacity. Similarly, Abdallah et al. [
22] also found that the anterior SSB was not inferior to the ISB for postoperative pain control. However, the analgesic effects of posterior SSB are inferior to those of ISB, with high pain scores at 6 and 12 hours on movement. These results are similar to findings from other studies [
12,
13]. More patients in the ISB group than in the SSB group required postoperative oxycodone, although there was no statistically significant difference in first 24-hour oxycodone consumption. We postulate that this might be due to rebound pain associated with ISB. As the ISB is a very dense block, patients may experience severe pain when the block wears off [
23]. This could be another advantage of the SSB block, where studies have shown that patients have a smoother transition and less rebound pain than with ISB [
24].
As the axillary nerve contributes about 10% of innervation to the shoulder, some authors have suggested combining the SSB with an axillary block [
12,
13]. In our study, we found that many patients who received SSB also experienced blockade of the axillary nerve, especially in the anterior SSB group (up to 75%). This could be due to the retrograde spread of local anesthetic to the posterior division of the upper trunk, which gives rise to the axillary nerve [
25]. In HannaŌĆÖs study [
26], the branching pattern in the upper trunk included the suprascapular nerve, posterior division, and anterior division. The posterior division is more closely related to the suprascapular nerve rather than the anterior division. Thus, it may be unnecessary to perform an axillary block to supplement the anterior SSB.
A known disadvantage of an ISB is having an insensate limb, which may be distressing to some patients and can result in injury to the limb. We found that the SSB can be quite selective in blocking the suprascapular nerve and axillary nerve. Hence, performing an SSB will minimize the risk of developing an immobile and insensate limb. Other adverse effects associated with an ISB, such as HornerŌĆÖs syndrome and hoarseness of voice, can also be avoided with an SSB.
While it is not currently routine practice, we should consider doing bedside spirometry for patients prior to performing an ISB. It would be advisable to avoid ISB in patients with compromised lung function who are unable to tolerate a further 30% reduction. In this study, none of the patients experienced dyspnea/desaturation since we excluded patients with obesity or pre-existing lung disease. The baseline spirometry values of all our patients were within the normal range.
As we wanted to avoid performing sham blocks, we were unable to blind our patients. However, the principal anesthesiologists and outcome assessors were blinded. Another limitation was that we performed single-shot blocks with 0.5% ropivacaine and the effect might have worn off by 24 hours. We tried to overcome this limitation by assessing outcomes at 1, 6, 12, and 24 hours. Our study did not capture long-term outcomes.
In conclusion, anterior SSB was found to better preserve pulmonary function than ISB and there were no statistically significant differences in their analgesic effects. In addition, anterior SSB also had fewer adverse effects, such as HornerŌĆÖs syndrome, hoarseness of voice, and dense motor blockade, than ISB. Therefore, we recommend performing anterior SSB in patients undergoing arthroscopic shoulder surgery, especially in the patients at high risk of respiratory compromise.