Anesthetic management of geriatric patients
Article information
Abstract
The number of elderly patients who frequently access health care services is increasing worldwide. While anesthesiologists are developing the expertise to care for these elderly patients, areas of concern remain. We conducted a comprehensive search of major international databases (PubMed, Embase, and Cochrane) and a Korean database (KoreaMed) to review preoperative considerations, intraoperative management, and postoperative problems when anesthetizing elderly patients. Preoperative preparation of elderly patients included functional assessment to identify preexisting cognitive impairment or cardiopulmonary reserve, depression, frailty, nutrition, polypharmacy, and anticoagulation issues. Intraoperative management included anesthetic mode and pharmacology, monitoring, intravenous fluid or transfusion management, lung-protective ventilation, and prevention of hypothermia. Postoperative checklists included perioperative analgesia, postoperative delirium and cognitive dysfunction, and other complications. A higher level of perioperative care was required for older surgical patients, as multiple chronic diseases often makes them prone to developing postoperative complications, including functional decline and loss of independence. Although the guiding evidence remains poor so far, elderly patients have to be provided optimal perioperative care through close interdisciplinary, interprofessional, and cross-sectional collaboration to minimize unwanted postoperative outcomes. Furthermore, along with adequate anesthetic care, well-planned postoperative care should begin immediately after surgery and extend until discharge.
Introduction
The WHO’s ‘World Report on Aging and Health’ revealed significant impairments in the elderly population in Europe, and the number of elderly people is expected to double by 2050 [1]. As the population of a country continues to age, the demands for surgical services increase. Elderly patients often require a higher level of care than younger patients do during the perioperative period, with higher health care costs. Strategies to optimize anesthesia care to reduce complications and improve outcomes in elderly surgical patients will also be of great value to the individual patients and society.
This article reviews the perianesthetic considerations for geriatric patients according to three conceptual categories: preoperative considerations, intraoperative management, and postoperative problems. It also aims to establish a framework to assess the complex issues related to the perioperative care of elderly patients.
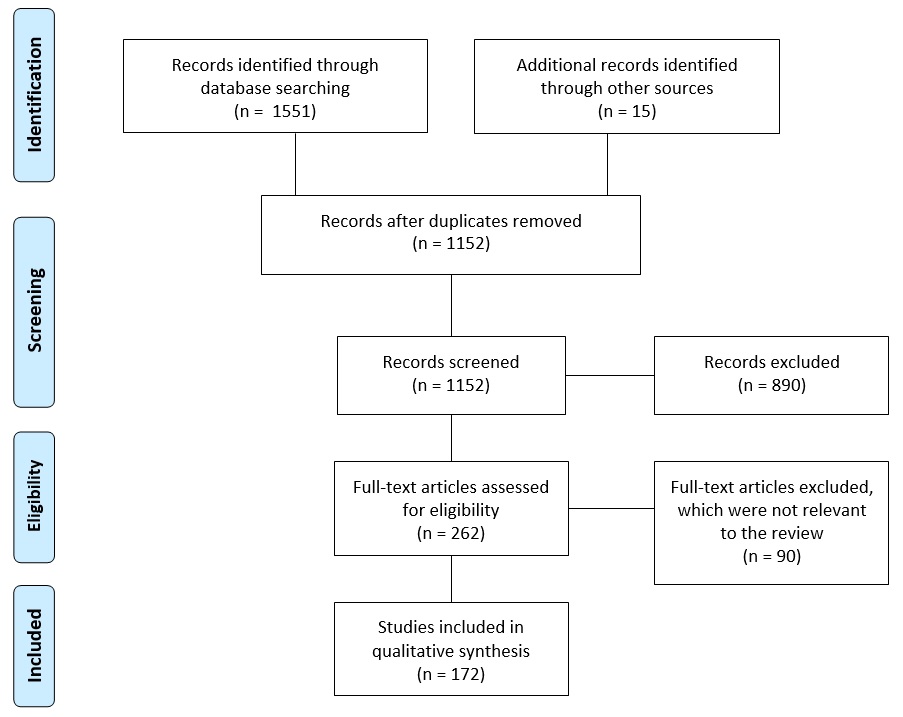
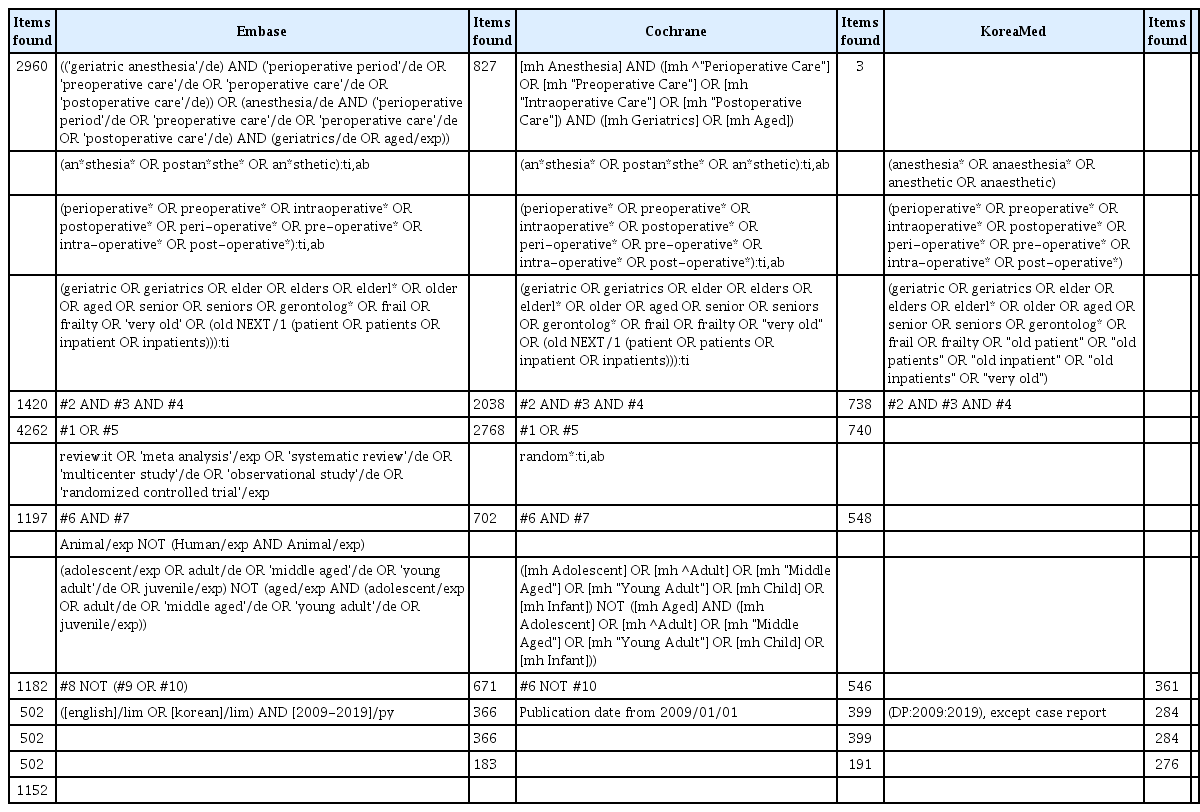
The authors performed a comprehensive literature review based on major international databases (PubMed, Embase, Cochrane) and a Korean database (KoreaMed) to identify systematic reviews, meta-analyses, practice guidelines, and clinical trials published in the last 10 years (Appendix 1). The initial search resulted in 1,551 citations and an additional 15 articles were obtained by a manual search through the related references. Of these, the authors selected 262 publications, which were further narrowed to 172 based on strength of evidence, relevance to geriatric patients, and focused on the perioperative period (Fig. 1).
Preoperative Management
Assessment of functional reserve
Comprehensive geriatric assessment (CGA) in the preoperative period include systematic evaluation of comorbidities, functional status, neurocognitive function, sensory impairment, substance abuse, frailty, nutrition, and medication. Preoperative CGA has a positive impact on postoperative outcomes in older patients undergoing elective surgery [2]. A recent Cochrane review including 1,583 hip fracture surgeries in subjects ≥ 65 years showed that CGA probably reduces mortality (risk ratio [RR] 0.85, 95% CI 0.68–1.05) and referral to an increased level of care (RR 0.71, 95% CI 0.55–0.92) [2]. However, CGA may make little or no difference in major postoperative complications and delirium rates [3]. Physicians must therefore recommend their patients to undergo all the appropriate preoperative evaluations and interventions such that they can improve their functional reserve and make an informed decision [4,5]. Furthermore, anesthesiologists are strongly encouraged to get involved in national surveys and clinical outcomes research focused on elderly surgical patients [6].
Baseline functional status should first be evaluated in ambulatory patients using a simple screening test, followed by in-depth or full screening of basic and instrumental activities of daily living (ADL) [7,8]. The patient should be evaluated for limitations in gait and mobility using the Time Up and Go (TUG) test [9,10]. In a 2018 prospective cohort study among 131 patients ≥ 65 years old who underwent elective major surgery for cancer, those who were dependent in ADLs and had an unfavorable TUG test had a significantly higher 1-year mortality (odds ratio [OR] 4.5, 95% CI 1.21–18.25, P = 0.034) than the other patients. As such, functional assessments such as ADL and TUG test as well as mild cognitive impairment are predictors of long-term outcomes in elderly cancer patients [11]. A 2005 prospective study of 120 patients ≥ 60 years old who underwent thoracic surgery also showed dependence in ADLs and impaired cognitive conditions as important predictors of postoperative complications [12].
Age-associated organ reserve decline, compounded by chronic diseases, also leads to high incidence of postoperative complications in the elderly patient, including neurologic, pulmonary, cardiac, and renal comorbidities. More data on the effectiveness of various components of the CGA are needed, but a 2018 meta-analysis showed that comorbidity (Charlson Comorbidity Index ≥ 3), polypharmacy (≥5 drugs/day), and ADL dependency were predictive factors for postoperative complications in gastrointestinal cancer patients [13,14]. A more independent preoperative functional status strongly predicts better postoperative function and shorter recovery period after major abdominal surgery [15]. Using the one million longitudinal health insurance database in Taiwan, another 2017 retrospective study of patients ≥ 65 years old who received anesthesia showed that the leading comorbidity contributing to postoperative mortality is chronic renal failure (OR = 2.806), acute MI (OR = 4.58), and intracranial hemorrhage (OR = 3.758) [16].
The American College of Surgeons (ACS) and the American Geriatrics Society (AGS) together recently proposed a framework for routine multidomain preoperative assessment of geriatric patients. The ACS and AGS are also developing best practice guidelines for optimal perioperative care in geriatric surgical patients [17,18]. One component of this collaboration is the initiation of patient preparation (prehabilitation) before hospital admission through measures including, e.g., correction of any deficiency states, optimization of chronic drug treatment, and respiratory training [19].
Neurocognitive and behavioral assessment
Dementia has a prevalence of 5% to 8% among people ≥ 65 years old and may affect more than one third of individuals > 85 years [20]. As the geriatric population grows, the number of people living with dementia is projected to rise dramatically [21]. A 2018 meta-analysis study showed that the mortality of patients with dementia who underwent hip fracture surgery was increased 1.57, 1.97, 1.77, and 1.60-fold after a 30-day, 6-month, 1-year, and > 1-year follow up, respectively [22]. A 2014 retrospective cohort study of 45,602 aged patients who had a hip fracture also showed that dementia was associated with an increased risk of long-term care admission (hazard ratio [HR] 2.49, 95% CI 2.38–2.61, P < 0.001), higher mortality (HR 1.47, 95% CI 1.41–1.52, P < 0.001), and poor prognosis [23].
The recent ACS-AGS Guidelines for Optimal Preoperative Assessment of the Geriatric Patient include a routine preoperative neurocognitive assessment before surgery. For patients without a known history of cognitive impairment, “Mini-Cog” [24] is recommended as a short, easily applicable, and well-studied tool. Careful documentation of the patient’s preoperative cognitive status is critical for diagnosing and anticipating common postoperative complications such as postoperative delirium (POD) or cognitive dysfunction (POCD). Preexisting cognitive impairment predicts POD [25,26]. Postoperative cognitive impairment is associated with longer hospital stay, increased mortality, and functional decline. Explanations may be that patients with impaired cognition are less likely to engage in postoperative aggressive pulmonary hygiene and ambulation, causing a high risk of developing postoperative complications such as pneumonia, deep vein thrombosis, stroke, and cerebrovascular accident with neurologic deficit.
Cardiac evaluation
Diminished cardiac reserve in elderly patients often manifests as exaggerated drops in blood pressure during induction of general anesthesia (GA). Reductions in the responsiveness of beta-receptors caused by a beta-blocked state limits patients’ ability to increase cardiac output and properly respond to blood losses. Baroreceptor dysfunction and reduced responsiveness to angiotensin II further limit responsiveness to hypovolemia. All these factors may be compounded by comorbid myocardial ischemia related to atherosclerosis.
Assessing the metabolic equivalents (METS) of daily activities is a useful way to assess exercise tolerance for patients who may not participate in regular exercise. Geriatric patients should undergo cardiac tests and risk stratification and evidence-based optimization strategies should be applied before surgery [27]. The web-based ACS National Surgical Quality Improvement Program (NSQUIP) Risk Calculator is one of the recommended tools in the 2014 American College of Cardiology/American Heart Association Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery [27] . However, critical knowledge gaps remain for informed decision-making and recommendations targeting older patients. A 2016 study highlighted a critical need for large population-based studies including a broad spectrum of older patients [28]. A 2002 prospective study of 513 patients ≥ 70 years old undergoing non-cardiac surgery showed that abnormalities in preoperative electrocardiogram (ECG) are common but non-specific and thus are of limited value in predicting postoperative cardiac complications compared to the presence and severity of comorbidities [29]. Conversely, echocardiography may help provide insights into ventricular function and valve status; it may be considered in patients with significant cardiac comorbidities such as history of myocardial infarction (MI), congestive heart failure (CHF), or valvular heart disease.
Older patients are more vulnerable to perioperative cardiac adverse events. A 2018 retrospective study of 8,441 adult patients who underwent general and vascular surgeries showed that the underlying predictors of cardiac events after surgery included age > 65 years (OR 4.9, 95% CI 3.4–6.9, P < 0.01) [30]. In addition, a 2017 study showed one-year mortality in elderly patients undergoing hip fracture repair to be significantly higher in patients with postoperative atrial fibrillation, even in patients receiving anti-arrhythmic therapy [31]. The anesthesia-related cardiac arrest rate is a quality indicator to improve patient safety in the perioperative period. A 2017 systematic review showed that perioperative and anesthesia-related cardiac arrest rates only decreased with a country’s high Human Development Index (HDI), with perioperative cardiac arrest being 4-fold higher in geriatric patients in low-HDI countries compared to that in high-HDI countries [32]. Another 2014 study showed that a large majority of cardiac arrests in older patients were caused by not anesthesia-related factors. The major predictors of intraoperative cardiac arrests were poorer physical status as based on assessment guidelines from the American Society of Anesthesiologists (ASA) and the need for emergency surgery. All anesthesia-related cardiac arrests were medication-related or airway-related, highlighting the importance of preventive strategies [33].
Pulmonary evaluation
Pulmonary function declines with age due to loss of both lung and chest wall compliance and oxygen diffusion capacity, especially in smokers, contributing to decline in oxygen uptake and delivery. Age and functional dependence have been identified as the most reliable risk factors for postoperative pulmonary complications (PPC). A 2006 systematic review showed that patient-related risk factors for PPC included advanced age, ASA class 2 physical status or higher, functional dependence, chronic obstructive pulmonary disease, and CHF. In patients undergoing noncardiac surgery, the rates of PPC are 14% and 15% for ages ≥ 65 years and ≥ 70 years, respectively [34]. A 2017 prospective study for PPC, which included 1,202 patients showed that significant PPC risk factors, such as emergency (OR 4.47, 95% CI 1.59–12.56), surgical site (OR 2.54, 95% CI 1.67–3.89), and age (OR 1.03, 95% CI, 1.02–1.05) were nonmodifiable [35]. In addition, a 2003 prospective study of 517 patients ≥ 70 years old and undergoing noncardiac surgery showed that 31.7 percent of patients died from renal complications (HR 6.07, 95% CI 2.23–16.52, P < 0.001), cancer (HR 2.44, 95% CI 1.78–3.38, P < 0.001), and pulmonary complications (HR 2.41, 95% CI 1.30–4,48, P = 0.005). These studies showed that pulmonary complications were an independent predictor of mortality in elderly patients [36].
Depression
Senility alone is a high risk factor for depression, and the preoperative psychological burden that patients likely suffer may complicate the situation. ACS-AGS guidelines strongly recommend preoperative depression and substance abuse screening using a simple questionnaire [37]. More than 10% of elderly people have depressive symptoms significant enough to warrant clinical intervention [38]. A 2018 prospective cohort study of 1,035 individuals ≥ 70 years old who underwent transcatheter or surgical aortic valve replacement surgery showed that baseline depression (31.5 percent of patients screened positive) was associated with mortality after 1 month (OR 2.20, 95% CI 1.18–4.10) and 12 months (OR 1.532, 95% CI 1.03–2.24). Persistent depression 6 months after the procedure was associated with a 3-fold increase in mortality at 12 months (OR 2.98, 95% CI 1.08–8.20) [39]. Therefore, active multi-disciplinary management of these patients is needed perioperatively.
Frailty
Frailty is a syndrome of decreased physiologic reserve and resistance to stressors. According to the Cardiovascular Health Study, with 5,317 participants ≥ 65 years old, the overall prevalence of frailty in this community was 6.9%, with frailty increasing with age and being greater in women than men [40]. A prospective measure of frailty in 594 patients found that preoperative frailty was associated with an increased risk of postoperative complications (intermediately frail: OR 2.06; 95% CI 1.18–3.60; frail: OR 2.54; 95% CI 1.12–5.77), length of stay (intermediately frail: incidence rate ratio 1.49; 95% CI 1.24–1.80; frail: incidence rate ratio 1.69; 95% CI 1.28–2.23), and discharge to an assisted-living facility after previously living at home (intermediately frail: OR 3.16; 95% CI 1.0–9.99; frail: OR 20.48; 95% CI 5.54–75.68). Frailty independently predicted higher rates of postoperative complications in elderly patients [41]. In addition, a 2019 prospective cohort study of 326 geriatric patients who required emergency general surgery showed that a frail status increased the odds ratio of failure to rescue 3 times when compared with a nonfrail status [42]. A 2014 study including 275 subjects ≥ 65 years old showed that the multidimensional frailty score based on CGA is more useful than conventional methods like the ASA classification (area under the receiver operating characteristic curve, 0.821 vs. 0.647, P = 0.01) for predicting all-cause mortality rates in geriatric patients undergoing surgery [43]. According to a 2017 meta-analysis, sarcopenia and frailty seem to have significant adverse impacts on postoperative outcomes [44]. Another 2018 meta-analysis identified potentially modifiable prognostic factors (i.e., frailty, depressive symptoms, and smoking) associated with developing postoperative complications that can be targeted preoperatively to optimize care [45]. These results lend support to the view that intensive management of preoperative modifiable factors can prevent postoperative complications.
There is growing evidence that preoperative frailty in elderly patients is associated with increased adverse outcomes after surgery. Although further studies are needed, frailty evaluation will be a useful preoperative risk-stratification tool in perioperative geriatrics [46]. Geriatric specialists will be able not only to make more extensive assessments but also to implement prior rehabilitation measures. Moreover, anesthesiologists should be aware of their role in patient preparation, maintaining or enhancing patient’s functional reserve to facilitate postoperative rehabilitation and discharge back into the society.
Nutrition
A 2015 meta-analysis showed that perioperative oral nutritional supplementation had a positive effect on serum total protein and led to fewer complications, such as wound, respiratory, and urinary tract infections, but did not have a positive effect on postoperative mortality [47]. Another clinical trial study showed that perioperative taurine supplementation attenuated postoperative oxidative stress in elderly patients with a hip fracture, but did not improve postoperative morbidity and mortality [48]. However, a 2016 review, which included 41 trials with a total of 3,881 participants, showed that oral multinutrient supplements started before or soon after surgery might prevent complications within the first 12 months after a hip fracture although no clear effects on mortality were seen [49].
Oral nutrition and supplementation counteracted the effects of poor appetite and illness. Prolonged preoperative fasting should be avoided (except in cases with an intraabdominal pathology). Yeniay et al. [50] measured preoperative fasting duration with respect to time of the day and its effect on vital parameters and ECG in elderly patients undergoing surgery under spinal anesthesia (SA). The fasting times were far longer than recommended, with 15-hour fasting being related to a transiently increased cardiac stress and mild hypothermia. Malnutrition is a frequent yet often overlooked problem in the surgical field.
Polypharmacy
Geriatric patients usually takes various medications, especially cardiovascular and central nervous system acting medications. When compared with younger adults, older people are more likely to have impaired renal function; therefore, it is critical to adjust dosage to prevent adverse effects. The risk of adverse drug reactions increases with the number of drugs taken, leading to more hospital stays [51]. A 2016 analysis of 272 elderly patients with consecutive hip fracture showed that the total number of medications at the time of discharge was predictive of rehospitalization (OR 1.08, 95% CI 1.01–1.17, P = 0.030) but not predictive of mortality [52]. Furthermore, a 2018 meta-analysis showed that comorbidity (Charlson Comorbidity Index ≥ 3) [13], polypharmacy (≥ 5 drugs/day), and ADL dependency were predictive factors for postoperative complications [14]. The ACS/AGS Best Practices Guidelines for the Optimal Preoperative Assessment of the Geriatric Surgical Patients recommended that whenever possible, nonessential medications should be discontinued perioperatively and the addition of new medications should be kept to a minimum [17,53].
For patients at risk of POD, new benzodiazepines [54] and meperidine should be avoided [55,56]. Antihistamine H1 antagonists and strong anticholinergic effective drugs should be cautiously prescribed [54,57]. According to American College of Cardiology/American Heart Association guidelines, beta-blockers are indicated for patients who are already on it or whose known coronary artery disease represents an immediate risk in vascular surgery [58-60]. Beta-blockers should be started days to weeks before elective surgery and titrated to a heart rate of 60 to 80 beats/min in the absence of hypotension. Preoperative statin should be started as soon as possible before surgery for patients who have known vascular disease. For patients undergoing noncardiac surgery and currently taking statins, statins should be continued [60].
Cholinesterase inhibitors (e.g., galantamine, rivastigmine, and donepezil), which are used to slow cognitive decline, was not associated with an increased risk of postoperative respiratory complications among older patients with dementia undergoing hip fracture surgery [61]. Cholinesterase inhibitors may interact with muscle relaxants, thereby prolonging the actions of succinylcholine, reversing the effects of non-depolarizing neuromuscular blocking agents, and leading to larger doses needed to achieve a proper degree of neuromuscular blockade [61,62].
Anticoagulation therapy
A 2016 population-based cohort study of 154,047 hip fracture patients showed that 33% of them used one or more antithrombotic on admission, with a higher proportion of men and a higher mean age [63]. In most cases, perioperative bridging anticoagulation is no longer recommended when using novel oral anticoagulants and vitamin-K antagonists [64]. However, this recommendation does not apply to patients at high risk of thromboembolism. Although the use of anticoagulants in the elderly is basically similar with that in younger patients, the reduced renal function frequently seen in elderly patients requires consideration.
Intraoperative Management
Anesthesia in elderly patients
A 2019 meta-analysis showed that postoperative morbidity and mortality increased with age [65]. However, a 2018 meta-analysis showed that laparoscopic hepatectomy is a feasible and safe alternative to open hepatectomy in elderly patients because of the lower rates of morbidity and favorable postoperative recovery and outcomes [66]. Another 2018 meta-analysis showed that the outcomes of laparoscopic gastrectomy for elderly gastric cancer patients were comparable to those in nonelderly patients. A 2017 study showed that laparoscopic liver resection of colorectal liver metastases in subjects ≥ 70 years of age is associated with a significant lower morbidity and a shorter stay [67]. The oncological outcomes were comparable with those in open liver resection even though the benefits of the laparoscopic approach appeared to fade with increasing age. Another recent retrospective study of patients ≥ 80 years old who underwent transabdominal preperitoneal repair of groin hernia showed that the incidence of postoperative complication was influenced by poor performance status, lower hemoglobin level, and lower albumin level rather than old age [68]. Therefore, age alone should not preclude laparoscopic gastrectomy in elderly patients [69].
However, whether old age itself is the only criterion for determining the indication of surgery remains controversial. A 2017 meta-analysis that included 18 studies of pancreaticoduodenectomy in patients ≥ 80 years old showed a higher 30-day postoperative mortality rate (OR 1.51, 95% CI 1.48–3.31, P < 0.001) and length of hospital stay (OR 2.23, 95% CI 1.36–3.10, P < 0.001) in this group of patients compared to that in younger patients. The overall postoperative complication rate was high (OR 1.51, 95% CI 1.25–1.83, P < 0.001) in aged patients [70]. Another recent prospective study including 165 patients who had pancreaticoduodenectomy showed that the 90-day mortality rate (5.9% in those ≥ 80 years old vs. 2% in the younger group, P = 0.335) and the postoperative complication rate (64.7% in the elderly vs. 62.8% in the younger group, P = 0.83) were similar, although the older patients were far more likely to be discharged to a rehabilitation facility than younger patients were (47.1% vs. 12.8%, P < 0.001) [71]. Careful selection of elderly patients and optimal perioperative care, rather than age, should be used to determine whether surgical intervention is indicated. Therefore, the question arises as to whether surgery is associated with a better outcome for the elderly patient when compared with conservative treatment. Ideally, individual parameters should be assessed at an interdisciplinary level, thereby preventing a complication-prone decision-making process based on surgical diagnosis. Once the decision to operate has been made, experienced staffs should be available at all times to anesthetize and operate on the patient as well as to organize appropriate postoperative care.
Mode of anesthesia
To date, there is insufficient evidence to support a single best anesthetic plan for elderly patients. No difference was found in postoperative morbidity, rates of rehospitalization, in-patient mortality, or hospitalization costs in geriatric patients undergoing regional anesthesia (RA) or GA for hip fracture repair [72,73]. GA and RA are both useful for older non-cardiac patients, but for some procedures, e.g., hip fracture surgery, RA seems the technique of choice. The mode of anesthesia may only play a secondary role in mobility, rehabilitation, and discharge delay. There are no specific recommendations regarding the preferred type of anesthesia for elderly non-cardiac patients [74]. Another 2014 population-based retrospective cohort study that included 6,135 age-matched adult pairs with dementia undergoing hip fracture surgery showed that GA and RA are associated with similar rates of most perioperative adverse events (GA, 11.3%; RA, 10.8%, P = 0.44) [75]. The mode of anesthesia also did not have any significant effects on perioperative outcomes (MI, pulmonary complication, stroke, urinary tract infection, and wound infection) after lower extremity amputation in a total of 3,260 geriatric patients [76]. While anesthesia preparation time, start time of surgery, length of surgery, time to sit, and time to walk were shorter in GA, time to fast-track eligibility, phase 1 recovery time, and time to discharge were similar among patients who received SA [77]. Another 2014 retrospective cohort study that included 56,729 patients ≥ 50 years old undergoing hip repair surgery found that RA was not associated with a lower 30-day mortality when compared with GA (RA, 5.4%; GA, 5.8%; instrumental variable estimate of risk difference, -1.1%, 95% CI -2.8 to 0.5), P = 0.20) but was associated with a modestly shorter length of stay. These findings do not support a mortality benefit for RA in this setting [78].
However, a recent retrospective study that included 16,695 geriatric patients and analyzed mortality within 90 days of undergoing hip fracture repair surgery showed that GA and conversion from RA to GA were associated with a higher risk of mortality (HR 1.22, 95% CI 1.11–1.35, P < 0.001) during hospital stay when compared with RA, but this higher risk did not persist after discharge. Furthermore, GA was associated with a higher risk of all-cause readmission when compared with RA, suggesting that RA may be preferable [79]. Another 2019 retrospective comparative study including 89 patients ≥ 70 years old undergoing major lumbar surgery showed that there was an association between epidural anesthesia and superior perioperative outcomes, such as episodes of hypertension and tachycardia during anesthesia and POD, nausea, vomiting, and pain [80]. A 2000 meta-analysis concluded that there were marginal advantages for RA when compared with GA for hip fracture patients in terms of early mortality and risk of deep vein thrombosis [81]. A 2014 review showed that multimodal drug therapy and RA can be effective for perioperative pain management in the elderly, although it did not improve long-term mortality [82].
Several ongoing large-scale randomized controlled trials (RCTs) should provide future guidance on the best anesthesia technique for hip surgery in the elderly [83-85]. Regardless of the type of anesthesia chosen, anesthesia should be carried out by experienced anesthesiologists who are trained to manage the perioperative care of geriatric patients [62,86]. Anesthesiologists should then base the choice of anesthetic on patient preferences, comorbidities, and potential postoperative complications.
A 2018 study of 392 older patients showed that propofol-based GA might decrease the incidence of delayed neurocognitive recovery at one week after surgery when compared with sevoflurane-based GA (propofol 14%; sevoflurane 23.2%; OR 0.577, 95% CI 0.342–0.975, P = 0.038) [87]. However, another recent study that included 28 RCTs with 4,507 participants found low-certainty evidence that maintenance with propofol-based total intravenous anesthesia (TIVA) or with inhalational agents may affect the incidence of POD, mortality, or length of hospital stay [88].
In elderly patients undergoing hip fracture repair, continuous spinal anesthesia (CSA) provided fewer episodes of moderate-to-severe hypotension when compared with a single intrathecal injection of 7.5 mg bupivacaine [89]. A prospective cohort study showed that cardiac output and blood pressure decreased significantly after the onset of SA in elderly patients, mainly due to a decrease in stroke volume and not in systemic vascular resistance [90]. A 2014 prospective randomized study of elderly high-risk patients undergoing hip replacement surgery showed that CSA and psoas compartment sciatic nerve block (PCSNB) produced a satisfactory quality of anesthesia. Fewer hemodynamic changes in PCSNB cases when compared with CSA cases were also noted [91]. A 2015 prospective randomized study comparing midazolam with propofol sedation in hypoalbuminemia (albumin level below 3 g/dl) geriatric patients under SA found that when compared with midazolam, propofol is associated with greater hemodynamic stability, lesser respiratory depression, and faster recovery [92].
Anesthetic pharmacology
Standard anesthetic doses can cause more profound clinical effects in the elderly, because of differences in pharmacokinetics and pharmacodynamics with the general population. Lower doses are required for propofol, remifentanil, ropivacaine, and desflurane [93]. Particular care should be taken with hypnotic agents, as the dose required to induce anesthesia is lower but the onset time is prolonged [94]. Depth of anesthesia monitoring is recommended [95,96]. Anesthesiologists should be familiar with potentially inappropriate medications for older patients according to Beers criteria. Thus, for example, elderly people have increased sensitivity to benzodiazepines and decreased metabolism of long‐acting agents; in general, all benzodiazepines increase the risk for cognitive impairment, delirium, falls, fractures, and motor vehicle crashes in elderly people [53].
Neuromuscular blocking and reversal agents
The dose of neuromuscular blocking agents (NMBAs) should hardly be reduced in the elderly for intubation, but their duration of action is often prolonged and difficult to predict along with age-induced changes in pharmacokinetics of long and intermediate-acting NMBAs (especially, aminosteriods including rocuronium and vecuronium), which may cause postoperative residual neuromuscular blockade and associated complications. Therefore, perioperative neuromuscular monitoring including a train-of-four monitoring is strongly recommended [97] .
Benzylisoquinoliniums including atracurium and cisatracurium have more reliable durations of action because they depend less on renal and hepatic function for their elimination and can thus be favorably considered for use in the elderly [98]. Neostigmine and pyridostigmine are preferable to edrophonium as NMBA reversal agents because their prolonged duration of action can counterbalance that of NMBAs; however, neostigmine reversal may be ineffective or prolonged and standard doses of sugammadex are required in the elderly [93,98].
Monitoring
The professional association of anesthesiologists recommends routinely considering using the following monitoring devices for the elderly, particularly during major or emergency surgery [6].
For intra-arterial blood pressure monitoring, hemoglobin concentration, blood glucose, arterial blood gas testing, and beat-to-beat blood pressure monitoring are recommended. A suitable limit of blood pressure is a fall in systolic blood pressure of more than 20% from pre-anesthesia induction baseline.
For central venous monitoring, catheterization may provide an additional route of venous access after complex surgery when vasoactive drug support is necessary, but its use should be balanced against the possible complication of the procedure. For cardiac output monitoring, there is still limited evidence in the elderly. Because elderly patients have poorly compliant aortas, cardiac output monitoring using Doppler directed at the aorta may provide less accurate information.
For cerebral oxygen saturation, an episode of a decrease in regional cerebral oxygen saturation (rSO2) of more than 15% of the baseline value is indicative of cerebral ischemia. Ružman et al. [99] evaluated the changes of rSO2 measured by near-infrared spectroscopy during elective laparoscopic cholecystectomy under TIVA and the association between patient characteristics and critical decline in rSO2. The rSO2 was significantly lower in patients older than 65 years, suggesting that monitoring of cerebral oxygenation could be an important part of the perioperative care to prevent cerebral hypoxia in older patients. In addition, early evidence suggests that monitoring of cerebral oxygen desaturation and early intervention may reduce POD or POCD [100].
For depth of anesthesia monitoring, processed electroencephalogram (EEG) neuromonitoring including a bispectral index or entropy monitor is recommended to avoid excessive depth of anesthesia, thereby preventing the development of POD [95,96] or POCD [100] in elderly patients. Lastly, perioperative neuromuscular monitoring is strongly recommended to keep the proper degree of neuromuscular blockade and its safe reversal [97,101].
Fluid management and blood transfusion
Intraoperative fluid optimization may be associated with benefit in geriatric hip fracture patients. A 2015 systematic review showed that goal-directed fluid therapy during hip fracture repair under SA does not result in a significant reduction in length of stay or postoperative complications [102]. Discharge time was similar in the anesthetist-directed fluid therapy group and the pulse-contour-guided fluid optimization strategy group, as was total length of stay. A nested meta-analysis of 355 patients found non-significant reduction in early mortality (relative risk [RR] 0.66, 95% CI 0.24–1.79) and in-hospital complications (RR 0.80, 95% CI 0.61–1.05) when goal-directed intervention fluid therapy was implemented. However, the study provided preliminary evidence that goal-directed fluid therapy may have a mortality reduction benefit. A 2014 systematic review including 734 high-risk patients aged 50 years or older found that the use of a cardiac output-guided hemodynamic therapy algorithm did not reduce a composite outcome of complications or 30-day mortality when compared with the usual standard of care [103].
In high-risk surgical patients, several studies have demonstrated that goal-directed hemodynamic therapy (GDHT) significantly reduced postoperative mortality and morbidity [104,105]. However, several studies found that GDHT was not associated with improved cardiac performance and exerted a statistically uncertain risk reduction in postoperative complications in elderly patients [102,106]. Subsequently, a 2016 RCT in patients aged ≥ 70 years old undergoing hip-fracture surgery also indicated that the main GDHT component, the stroke volume maximization by fluid challenges, and traditional pre-anesthesia fluid loading are of questionable value in the elderly [107]. A multicenter RCT involving 807 patients ≥ 75 years old and using a stepped wedge cluster design to assess the effectiveness of an optimization strategy involving GDHT, lung-protective ventilation, and depth of anesthesia monitoring for GA on postoperative morbidity and mortality in high-risk elderly patients undergoing high-risk surgeries (the OPTI-AGED study) identified a considerable gap between clinical practice and the relevant guidelines for anesthetic optimization [108]. Implementation of such multimodal optimization strategies varied independently of factors related to the population or type of surgery, and thus, potential benefit should be further addressed in elderly patients [109].
To date, it is still controversial whether red blood cell (RBC) transfusions might increase the risk of infection after hip fracture surgery in geriatric patients. The Transfusion Requirements In Frail Elderly (TRIFE) randomized study with 284 patients showed that a more liberal RBC transfusion strategy (Hb < 11.3 g/dl 7 mmol/L) was not associated with higher infection risk in subjects undergoing hip fracture surgery compared to the restrictive RBC strategy group (hemoglobin [Hb] < 9.7 g/dl; 6 mmol/L). The rate of infection was 72% in the restrictive RBC strategy group compared with 66% in the liberal group (RR 1.08, 95% CI 0.93–1.27, P = 0.29) [110]. A 2015 Cochrane review of 2,722 participants between 81 and 87 years old undergoing hip fracture surgery provided preliminary evidence for similar mortality, functional recovery, or postoperative morbidity when using the thresholds for RBC transfusion in the liberal strategy (aiming to maintain a Hb level usually around 10 g/dl) versus the restrictive strategy (based on symptoms of anemia or a lower Hb concentration usually around 8 g/dl) [111]. A 2015-nested analysis in the Transfusion Requirements After Cardiac Surgery (TRACS) RCT focusing on 30-day all-cause mortality and severe morbidity showed no difference between liberal and restrictive transfusion strategy inpatients aged less or more than 60 years old. However, there was an increased rate of cardiogenic shock in the elderly patients in the restrictive transfusion strategy group [112]. A 2019 prospective, multicenter, controlled trial randomizing 2,470 elderly (≥ 70 years) patients undergoing non-cardiac surgery is now to evaluate whether a liberal transfusion strategy (defined as the transfusion of a single RBC unit when Hb is < 9 g/dl with a subsequent target range of 9–10.5 g/dl) reduces the major adverse events after non-cardiac surgery compared to a restrictive strategy (transfusion of a single RBC unit when Hb < 7.5 g/dl with a subsequent target range of 7.5–9 g/dl) within 90 days after surgery [113].
Another 2019 RCT showed that salvaged autologous blood leukocyte filtration could improve ventilation, promote oxygenation and gas exchange, and inhibit lung inflammatory and oxidative stress reactions in elderly patients undergoing lumbar spinal surgery [114].
Lung-protective ventilation
The ACS best practice guidelines for PPC detailed risk factors and strategies to prevent complications. A 2018 expert survey including 362 respondents suggested a care bundle composed of factors before surgery, i.e., supervised exercise programs and inspiratory muscle training; factors during surgery, i.e., low tidal volume ventilation (6–8 ml/kg) with individualized positive end-expiratory pressure (PEEP) of 5–8 cmH2O and repeated recruitment maneuvers, use of routine monitoring to avoid hyperoxia, and efforts to limit neuromuscular blockade; and post-operative factors, i.e., deep breathing exercises and elevation of the head of the bed [115].
Prevention of hypothermia
Elderly patients are vulnerable to perioperative hypothermia, leading to increased morbidity. Especially, during transurethral resection of the prostate (TURP) or bladder tumor (TURB) under SA or GA, or arthroscopic shoulder surgery under GA, it is important to maintain a normal range of body temperature throughout the whole perioperative period. Many studies have therefore been performed to investigate the effects of various active or passive warming devices and methods including a forced‐air warming blanket or heated humidifier circuit on perioperative hypothermia or shivering in elderly patients undergoing TURP or TURB under SA or GA and arthroscopic or open urologic surgeries under GA [116-119]. Jo et al. [116] suggested that a brief period of preoperative forced-air warming did not significantly reduce the incidence of intraoperative hypothermia, but it could significantly reduce its severity in elderly male patients undergoing TURP under SA. Moreover, Zhang et al. [120] reported that use of a forced-air warming system combined with an electric blanket was a more effective method for maintaining body temperature compared to individual devices alone in elderly TURP patients.
Hong et al. [117] reported that warming blanket application for 10 min before induction of anesthesia reduced the incidence of hypothermia as measured one hour after induction compared to one-layer cotton blanket. A prospective observational study showed a heated humidifier was more effective in preventing intraoperative hypothermia in elderly patients undergoing open urologic surgeries than a heat moisture exchanger was [118]. A retrospective study performed in arthroscopic shoulder surgery reported that the incidence of postoperative hypothermia was higher and the associated temperature drop was more prominent in geriatric patients compared to young adult patients and suggested that additional warming methods are needed to prevent perioperative hypothermia in geriatric patients [119]. Altogether, these and other studies demonstrated that various warming strategies could be helpful in keeping the body temperature stable in elderly patients undergoing surgery under GA or RA.
Postoperative Management
Postoperative adverse outcomes
Despite the prevalence of preoperative chronic medical conditions, most patients do well postoperatively. Nonetheless, in a prospective cohort study of 544 patients aged 70 and older undergoing non-cardiac surgery, an overall 21 percent of patients developed adverse outcomes and 3.7% died during the in-hospital postoperative period. ASA physical classification, emergency surgery, and intraoperative tachycardia increased the odds of adverse events [121]. Another prospective study of 517 patients ≥ 70 years old and undergoing non-cardiac surgery showed that 31.7 percent of patients were deceased at the time of follow-up and a history of cancer (HR 2.44, 95% CI 1.78–3.38, P < 0.001), ASA physical status > 2 (HR 2.27, 95% CI 1.61–3.21, P < 0.001), neurologic disease (HR 1.59, 95% CI 1.13–2.24, P = 0.008), age (HR 1.42 per decade, 95% CI 1.11–1.81, P = 0.005), postoperative pulmonary complication (HR 2.41, 95% CI 1.30–4.48, P = 0.005), and renal complication (HR 6.07, 95% CI 2.23–16.52, P < 0.001) were all significant independent predictors of decreased long-term survival [122]. Co-morbid conditions, age, and new hospitalization after discharge were important independent predictors of a long-term decrease in quality of life. To improve postoperative long-term quality of life, geriatric surgical patients should be evaluated for their potential pre- and intra-operative risk factors.
Postoperative transfusion
In a 2016 RCT including 284 frail elderly patients undergoing surgical hip fracture, postoperative transfusion using the liberal hemoglobin target (7 mmol/L, or 11.3 g/dl) improved survival within one year after surgery in the frailest elderly (the nursing home residents) without impairing recovery from physical disabilities and overall quality of life or increasing the risk of infection when compared with the restrictive hemoglobin target (6 mmol/L, or 9.7 g/dl) [123]. According to the Hb thresholds, recovery from physical disabilities in frail elderly hip fracture patients was similar after a restrictive RBC transfusion strategy (Hb < 9.7 g/dl; < 6 mmol/L) and after a liberal strategy (Hb < 11.3 g/dl; < 7 mmol/L). The 90-day mortality rate was higher for the nursing home residents in the restrictive transfusion group (36%) than for those in the liberal group (20%) (HR 2.0, 95% CI 1.1-3.6, P = 0.010). Implementation of a liberal RBC transfusion strategy in nursing home residents has thus the potential to increase survival [124].
Perioperative analgesia
Elderly patients are often undertreated for pain. Acute pain management in the elderly is challenging, with physiological frailty, medical comorbidities, and cognitive impairment commonly compounding pain assessment and treatment. A 2003 retrospective cohort study including 8,855 subjects aged 16 years and older showed that the risk of respiratory depression after short-term opioids use increased with age, substantially after 60 years of age [125]. A 2014 review suggested that multimodal drug therapy and perioperative regional analgesia can be very effective for perioperative pain management in elderly patients [81]. Paracetamol is safe and considered first-line therapy. Nonsteroidal anti-inflammatory drugs should be used with caution because they can cause gastric and renal damage. Although morphine is effective, cautious administration to elderly patients with poor renal or respiratory function and impaired cognition must be taken into consideration.
RA as part of multimodal perioperative treatment can often reduce postoperative neurological, pulmonary, cardiac, and endocrine complications. RA or analgesia has not been proven to improve long-term morbidity but does benefit immediate postoperative pain control. In addition, multimodal drug therapy utilizes a variety of nonopioid analgesic medications in order to minimize dosage and prevent adverse effects from opioids while maximizing analgesic benefit [81]. A 2018 review showed that comprehensive pain protocols for elderly hip fracture patients are required, with fascia iliaca blocks as a local anesthesia method of choice [126]. Ultrasound-guided regional anesthesia/analgesia is an important part of anesthesia practice in the elderly population, the growth of which will continue to outpace that of the younger population due to improvements in lifespan worldwide [127]. In a 2016 RCT comparing ultrasound-guided continuous femoral nerve block versus continuous fascia iliaca compartment block in 60 elderly patients undergoing hip replacement surgery, both ultrasound-guided blocks provided effective anesthesia and postoperative analgesia [128]. Moreover, in a 2014 RCT comparing the hemodynamic effects of combined PCSNB with CSA in elderly high-risk patients undergoing hip replacement surgery, PCSNB produced satisfactory-quality anesthesia in elderly high-risk patients with fewer hemodynamic changes compared with CSA [91].
Another RCT showed that after a major abdominal surgery in the elderly patient, patient‐controlled analgesia, regardless of the route (epidural or parenteral), was effective. Furthermore, patient-controlled epidural analgesia using local anesthetics and an opioid provided better pain relief and improved mental status and bowel activity when compared with intravenous patient-controlled analgesia [129].
Postoperative delirium
POD is a common serious postoperative complication, especially in older people, and is associated with increased mortality, morbidity, and health costs. The overall prevalence of delirium in older patients after surgery has been estimated to be 10% [130]. One study in which 144 patients > 50 years were scheduled for an operation requiring a postoperative intensive care unit (ICU) admission showed that 44 percent of patients developed delirium [131]. A recent review of 35 selected articles showed that the incidence of POD was up to 50% [132]. However, a 2015 study including 459 elderly patients found that incident POD was not significantly associated with decreased survival after hip fracture repair and that survival was a function of age at the time of surgery, illness severity based on ASA physical status, and duration of ICU stay after surgery [133].
Among the risk factors for POD, preexisting cognitive impairment and dementia are the strongest predisposing factors [131, 134]. A 2006 study including 333 elderly patients undergoing noncardiac surgery found that 46 percent of patients developed POD. By multivariate logistic regression, age (OR 2.5, 95% CI 1.5–4.2) and moderate (OR 2.2, 95% CI 1.2–4.0) or severe (OR 3.7, 95% CI 1.5–9.0) preoperative resting pain were important contributing factors [135]. Therefore, adequate opioid-reduced analgesia is of great importance. A 2019 review suggested that a clinical trial on the usefulness of the STOP-BANG questionnaire on obstructive sleep apnea as a preoperative stratification for POD showed no difference between the low-risk group and the intermediate-to-high risk groups in POD incidence, duration of delirium, and length of ICU. However, a higher preoperative risk for obstructive sleep apnea was associated with a 3-fold higher risk for POD and coma [136]. A retrospective study that included 318 elderly patients undergoing total knee arthroplasty also showed that preoperative dementia is the most important risk factor for POD, suggesting that those patients should be thoroughly evaluated and their dementia should be managed preoperatively. Adequate management of intraoperative hypotension and preoperative hemoglobin might also be helpful in reducing the incidence of POD [137].
A 2018 systematic review, which included 104 studies found no evidence of anesthesia types (GA vs. RA) influencing POD [138]. Another 2018 RCT, which included 256 patients ≥ 75 years old, found that Xenon anesthesia did not reduce the incidence of POD (Xenon; 9.7%, 95% CI 4.5–14.9, sevoflurane; 13.6%, 95% CI 7.8–19.5, P = 0.33) [139]. Meanwhile, a comparison of RA with GA on POD in elderly patients is underway in nine clinical trial centers in China with an expected total enrollment of 1,000 patients [84].
Intraoperative EEG waveform suppression, which often suggests excessive GA, has been associated with POD, prompting research on whether EEG-guided anesthetic administration decreases the incidence of POD. A 2019 systematic review for prevention of POD in elderly patients planned for elective surgery offered preliminary evidence that multicomponent interventions (i.e., comprehensive multidisciplinary care and multimodal interventions), antipsychotics, bispectral index-guidance, and dexmedetomidine treatment can successfully reduce POD incidence in elderly patients undergoing elective non-cardiac surgery [95]. However, recently, a remarkable large-scale RCT of 1,232 adults aged 60 years and older undergoing major surgery showed that EEG-guided anesthetic administration, compared with standard care, did not decrease the incidence of POD. This finding does not support the use of EEG-guided anesthetic administration for decreasing the incidence of POD [140]. Another 2019 RCT with 200 elderly patients undergoing hip fracture repair with SA supplemented with propofol sedation found that heavier intraoperative sedation was not associated with significant differences in mortality or return to pre-fracture ambulation up to one year after surgery [141]. Therefore, further large-scale and well-designed RCTs are needed to clarify the association between EEG-guided anesthetic administration or depth of anesthesia, and POD incidence.
A 2012 clinical trial that included 171 elderly subjects with hip fracture found that delirium episodes and cognitive decline during hospitalization were common, but inpatient geriatric consultation teams intervention reduced the incidence of POD (control group 53.2%; intervention group 37.2%; OR 1.92, 95% CI 1.04–3.54, P = 0.04). However, another study found that geriatric consultation had no effect on the severity or duration of POD episodes [142]. Although the results are not conclusive, a close collaboration with the geriatric team can be useful [143]. A 2017 meta-analysis that included 1,840 elderly patients concluded that comprehensive geriatric care may reduce the incidence of POD (OR 0.71, 95% CI 0.57–0.89, P = 0.003) [144].
Two systematic 2019 meta-analyses of RCTs showed that in elderly patients undergoing noncardiac surgery, perioperative administration of dexmedetomidine, compared with placebo, reduced the incidence of POD [145,146]. In contrast, a 2019 double-blinded, multi-center, randomized study that included 164 elderly patients undergoing cardiac surgery reported that dexmedetomidine-based GA resulted in reduced extubation time and postoperative morphine requirements when compared with propofol-based GA, but no significant difference was observed in POD incidence [147].
If possible, drugs that precipitate POD such as opioids, antihistamines, atropine, sedative hypnotics, and corticosteroids should be avoided in patients at risk, including benzodiazepine [54,148].
Postoperative cognitive dysfunction
POCD is another frequent neurologic complication occurring in geriatric patients. The type of anesthesia or analgesia and patient inflammatory response may contribute to POCD. A 2014 clinical trial that included 200 elderly patients with mild cognitive impairment showed that there is no difference in the incidence of POCD at 7 days after radical rectal resection under sevoflurane (33.3%) or propofol-based (29.7%) GA, even though sevoflurane had more severe impact on cognitive function than propofol [149]. However, a 2015 clinical trial that included 90 elderly patients scheduled for resection of an esophageal carcinoma showed the incidence of POCD was higher in sevoflurane than propofol anesthesia using the Mini Mental State Examination (MMSE) and the Montreal cognitive assessment (MoCA) scores. Furthermore, elevated plasma concentrations of TNF-α, interleukin (IL)-6, and S-100β protein were found in patients receiving sevoflurane anesthesia throughout the first postoperative week [150]. However, a 2016 RCT that included 80 elderly patients scheduled for a non-cardiac operation found a negative influence by sevoflurane anesthesia on the early (48 hours postoperatively) and late (9 months postoperatively) state compared to propofol anesthesia and no difference in inflammatory markers (IL6, IL10, TNF-α) between the two anesthesia groups [151]. A 2018 clinical trial that included 120 elderly scheduled for esophageal carcinoma resection showed that POCD incidence was higher in elderly patient receiving sevoflurane anesthesia while dexmedetomidine could alleviate POCD through decreasing TNF-α and IL-6 [152].
A 2018 RCT compared the effect of GA and SA on the occurrence of POCD up to postoperative 30 days in elderly patients undergoing hip fracture surgery and reported that the choice of anesthesia modality did not appear to influence the emergence of PCOD in the elderly patients [153]. Meanwhile, a 2019 RCT with 80 elderly patients undergoing orthopedic surgery concluded that compared with GA, SA can effectively reduce eye opening and language presentation times and also has few negative impacts on the short-term cognitive function and mental status of elderly patients, along with lower incidence of POCD [154].
A 2017 RCT was performed to observe whether combined GA and RA affected perioperative cognitive trajectory compared to only GA in elderly patients with arthroplasty [155]. Postoperative MMSE was significantly higher in the combined anesthesia group as well as significantly improved compared with preoperative MMSE score in both groups. Combined GA and RA protected perioperative cognitive trajectory, providing evidence supporting the combined use of RA and GA in elderly orthopedic patients vulnerable to POCD.
A 2016 meta-analysis including 13 RCTs of GA showed that dexmedetomidine significantly reduced the incidence of POCD (RR 0.59, 95% CI 0.45–2.95) and improved the MMSE score (mean difference [MD] 1.74, 95% CI 0.43–3.05) on the first postoperative day and reduced the incidence of POCD thereafter (MD 2.73, 95% CI 1.33–4.12) [156]. Another 2019 meta-analysis including 26 RCTs found that perioperative dexmedetomidine treatment significantly reduced the incidence of POCD (pooled ORs 0.59, 95% CI 0.45–2.95) and improved MMSE score (standardized mean difference [SMD] 1.74, 95% CI 0.43–3.05) on the first postoperative day and decreased IL-6 (SMD: -1.31, 95% CI: -1.87 to -0.75, P < 0.001) and TNF-α (SMD: -2.14, 95% CI: -3.14 to -1.14, P < 0.001) when compared with saline treatment [157]. A 2016 clinical trial with 134 elderly patients undergoing total knee arthroplasty found that parecoxib sodium decreased POCD incidence and plasma IL-1β, IL-6, and TNF-α levels, suggesting that parecoxib may influence POCD incidence through suppression of inflammation and pain [158]. Another clinical trial in 2017 that included 152 elderly patients scheduled for shoulder arthroscopy showed that parecoxib sodium pretreatment combined with dexmedetomidine could reduce the incidence of early POCD and yielded higher jugular venous oxygen partial pressure and jugular venous oxygen saturation values at postoperative day one when compared with the control group. This effect may be related to the improvement of postoperative analgesia and cerebral oxygen metabolism [159].
In a prospective randomized double-blinded controlled study, the effect of remifentanil and fentanyl on POCD and cytokine levels were investigated in elderly patients undergoing major abdominal surgery. The two opioid groups were comparable in terms of POCD incidence; however, IL‐6 levels were lower at the seventh day after surgery in the remifentanil group, suggesting that remifentanil did not reduce POCD compared to fentanyl [160].
Enhanced inflammation response has been increasingly reported in association with POCD [161]. Glucocorticoid receptor (GR) signal plays a key role in suppression of inflammation. In a 2010 prospective cohort that included 126 elderly patients undergoing hip fracture surgery with GA, plasma cortisol levels and the expression levels of GR and FK506 binding protein 51 (FKBP51) in leukocytes were determined from one day before surgery and to up to seven days after surgery. When compared with non-POCD patients, visual analogue scale (VAS) scores at 12 hours after surgery were higher in POCD patients. No significant difference in expression levels of GR was found between POCD and non-POCD patients, but high expression of FKBP51 in leukocytes and glucocorticoid resistance were associated with POCD in aged patients following hip fracture surgery [162].
A 2017 RCT reported that preoperative oral melatonin supplementation might improve early POCD in elderly patients undergoing hip arthroplasty, suggesting that the restoration of normal circadian function with good sleep quality may be a key factor in preventing or treating POCD [163].
To manage POCD, care bundles and protocols for the perioperative period may improve outcomes in the elderly patient. However, to date, there is no clear strategy to improve POD or POCD. Preventive strategies, early recognition, and management of perioperative risk factors seems to be the best modality to treat POCD until further progress is made [164]. Meanwhile, in Germany, a stepped-wedge cluster randomized (PAWEL) trial for the reduction of delirium and POD risks after elective procedures in adults > 70 years old is now planned with an expected 1,500 patients to enroll. Results of the trial should form the basis of future standards for preventing delirium and POCD in surgical wards [165].
Prevention of postoperative pulmonary complications
Pulmonary complications increase the risk of mortality after surgery and age is a significant risk predictor of pulmonary complications [34,166]. A large retrospective cohort study that included 8,920 elderly patients with hip fracture repair patients found that cardiac and pulmonary complications were most frequent (8% and 4% of patients, respectively) [167].
Well-documented risk factors for pulmonary complications include atelectasis, pneumonia, and pulmonary thromboembolism, advanced age, poor general health status, current infections, pre-existing cardiopulmonary diseases, hypoalbuminemia, and renal dysfunction. Interventions such as lung expansion maneuvers and thromboprophylaxis are effective in reducing the risk of pulmonary complications [168]. According to a 2006 systematic review that included 20 RCTs and 11 meta-analyses not limited to the elderly patient, lung expansion therapy (i.e., incentive spirometry, deep breathing exercises, and continuous positive airway pressure) reduces postoperative pulmonary risk after abdominal surgery. Well-designed trials are needed to clarify the magnitude of benefit and the comparative effectiveness of different modalities [169].
In a 2019 RCT with 76 elderly patients scheduled for hip joint surgery investigating whether pressure-controlled ventilation-volume guaranteed (PCV-VG) may result in better lung ultrasound score (LUS) by reducing atelectasis in the dependent areas of the lung and minimizing respiratory deterioration after surgery in elderly patients compared with volume-controlled ventilation (VCV), PCV-VG showed better LUS results as well as higher dynamic compliance and lower inspiratory peak pressure compared to VCV [170].
Prevention of urinary tract infections
In a 2019 retrospective cohort study in which 221 female patients (age 85.3 ± 7.0 years) with a history of hip surgery, urinary retention occurred in 34 out of the 221 cases (15.4%) and was significantly associated with cognitive impairment (OR 4.11, 95% CI 1.53–11.03, P = 0.005) and ADL (OR 2.61, 95% CI 1.11–6.18, P = 0 .029), under adjustment with age and body mass index (BMI). This study demonstrated that cognitive function and ADL were important risk factors for urinary retention, and suggested that the postoperative management of urinary retention is important when considering neurofunctional assistance and nursing care in daily living, especially in elderly female patients undergoing surgery after femoral neck and trochanteric fractures [171]. A 2014 clinical study of risk factors for urinary retention including 72 female elderly patients undergoing hip surgery showed that the early removal of the urethral catheter (per 1-day indwelling period increase, OR 0.33, 95% CI 0.11–0.96, P = 0.04) and preoperative dementia and/or delirium (OR 10.4, 95% CI 1.21–89.2, P = 0.03) had significant correlations with postoperative urinary retention. Femoral neck fractures and the surgical procedure used for the hip surgery did not induce damage to the bladder and nerves involved in voiding function, with the voiding function being recovered in all the patients after short-term intermittent catheterization [172]. Older adults are at particular risk for urinary tract infection, and indwelling urinary catheters should not be used as a substitute for adequate nursing care of incontinent patients.
Conclusion
The main aims of effective perioperative care in elderly patients are to improve the likelihood of them returning to their pre-morbid conditions and maintaining their presence in the community. The perioperative care of elderly patients requires optimization through a multidisciplinary approach that includes risk stratification models. However, the aforementioned approaches are time-consuming and remain a challenge in clinical routine because of limited human resources and lack of funding from healthcare systems. Moreover, the evidence base to inform perioperative care for elderly patients remains poor. More RCTs are needed to clarify the efficacy of GA versus RA for surgery. There are no clear care bundles and protocols, which improve POD or POCD. Preventive strategies and early recognition and management of perioperative risk factors seem to be the best modality until there is further progress in therapeutic interventions. Anesthetic techniques to manage appropriate hemodynamic status during the perioperative period to avoid ischemic complications are required. Anesthesiologists must participate in discussions on the utility of surgery and resuscitation and are strongly encouraged to participate in national surveys and outcomes research. We hope that health care practitioners will use this information to improve their daily practice and that additional research will be undertaken to further improve our future.
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Byung-Gun Lim (Conceptualization; Data acquisition and analysis; Investigation; Methodology; Writing–original draft; Writing–review & editing)
Il-Ok Lee (Conceptualization; Data acquisition and analysis; Investigation; Methodology; Supervision; Validation; Writing–original draft; Writing– review & editing)