|
 |
| Korean J Anesthesiol > Volume 72(6); 2019 > Article |
|
Abstract
Background
The supraglottic airway device is an appropriate alternative to tracheal intubation in laparoscopic surgery. We compared the Baska MaskŌōć with i-gelŌōć by measuring the oropharyngeal leak pressure (OLP) and hemodynamic and respiratory parameters during laparoscopic cholecystectomy.
Methods
A total of 97 patients were randomly allocated to either i-gel group (n = 49) or Baska Mask group (n = 48). Insertion time, number of insertion attempts, fiber-optic view of the glottis, and OLP were recorded. Heart rate, mean arterial pressure, peak airway pressure (PAP), lung compliance, and perioperative complications were assessed before, during, and after pneumoperitoneum.
Results
There were no significant differences between the two groups regarding demographic data, insertion time, fiber-optic view of the glottis, and the use of airway manipulation. The OLP was higher in the Baska Mask group than in the i-gel group (29.6 ┬▒ 6.8 cmH2O and 26.7 ┬▒ 4.5 cmH2O, respectively; P = 0.014). Heart rate, mean arterial pressure, PAP, and lung compliance were not significantly different between the groups. The incidence of perioperative complications was small and not statistically significant.
The supraglottic airway device (SAD) is an appropriate alternative to tracheal intubation because of its advantages such as stable hemodynamics and decreased airway morbidity. It also helps to maintain adequate ventilation in laparoscopic surgery, with increased peak airway pressure (PAP) under general anesthesia [1,2].
The i-gelŌōć (Intersurgical Ltd., UK) is widely used for laparoscopic surgeries [1,3ŌĆō5]. However, the Baska MaskŌōć (Logikal Health Products PTY Ltd., Australia), first introduced in 2012, provides more efficient ventilation by automatically inflating the cuff during positive pressure ventilation. The cuff differs from other non-inflatable cuffs in that it is continuous with the central channel of the device. As the pressure increases with positive pressure ventilation, the cuff automatically inflates and provides better oropharyngeal leak pressure (OLP) compared with that provided by existing SADs [6ŌĆō8]. However, there are only a few studies assessing the effectiveness of the Baska Mask. Therefore, the aim of this prospective randomized study was to compare the Baska Mask with the i-gel for suitability for laparoscopic surgery under general anesthesia with elevated PAP.
We tested our hypothesis that the Baska Mask would have a higher sealing pressure than the i-gel by comparing OLP (the primary outcome measure) between the two SADs in patients undergoing laparoscopic cholecystectomy. Further, we compared respiratory and hemodynamic variables, SAD insertion-related characteristics, and the incidence of postoperative airway complications between the two SADs.
This study was conducted on 100 patients, with American Society of Anesthesiologists physical status classification I or II, who underwent elective laparoscopic cholecystectomy under general anesthesia. Patients with a body mass index Ōēź 35, pregnant women, patients with gastroesophageal reflux disease, and patients who were expected to have difficult intubation were excluded from the study. Informed consent was obtained from each patient. After receiving approval from the Institutional Review Board of our hospital (DAUHIRB-18-186), this prospective study was registered at the Korea Clinical Research Information Service (permit number: KCT 0003428).
All patients fasted for 8 h before surgery. Routine monitoring, including electrocardiography, pulse oximetry, and bispectral index (BIS) (Aspect Medical Systems, USA) was initiated upon each patientŌĆÖs arrival at the operating room.
Oxygen (flow rate, 8 L/min) was delivered via a mask to all patients in the supine position. After preoxygenation, target-controlled infusion (TCI) of propofol and remifentanil, with an effect-site concentration (Ce) of 4 ╬╝g/ml and 5 ng/ml, respectively, was started to induce anesthesia using an OrchestraŌōć Base Primea device (Fresenius Kabi, France). After the loss of eyelid reflex and a BIS value < 50 were confirmed, a neuromuscular blockade was performed with rocuronium 0.8 mg/kg. The i-gel or Baska Mask was inserted when the train-of-four (TOF) count was zero.
During the operation, the Ce of TCI-propofol was adjusted to maintain a BIS value of 40ŌĆō60 [9], and the Ce of TCI-remifentanil was maintained to adjust the mean arterial pressure within the baseline value ┬▒ 20%. Rocuronium 0.15 mg/kg was also administered under peripheral neuromuscular monitoring. At the start of the operation, the following respiratory settings were used: inspired fresh gas at 3 L/min through the circle anesthesia breathing system, inspired tidal volume preset at 8 ml/kg, and inspiratory/expiratory ratio of 1 : 2. The respiratory rate was adjusted to maintain the end-tidal carbon dioxide (EtCO2) values at 30ŌĆō40 cmH2O [10]. At the end of the surgery, sugammadex was administered to counteract the effect of rocuronium as follows: if the TOF count was 0, sugammadex 4 mg/kg was administered; if the TOF count was 1ŌĆō4, sugammadex 2 mg/kg was administered.
The sizes of the i-gel and Baska Mask were chosen according to the patientŌĆÖs weight, considering the manufacturerŌĆÖs recommendations. Sizes 3 and 4 i-gel were used for patients weighing 30ŌĆō60 kg and 50ŌĆō90 kg, respectively [3]. According to the manufacturerŌĆÖs recommendations, sizes 3 and 4 Baska Masks are suitable for females or small males and average adult males, respectively [11]. However, we judged these criteria to be unclear. Thus, we decided to apply sizes 3 and 4 Baska Masks in patients with 30ŌĆō60 kg and > 60 kg body weights, respectively.
For inserting the i-gel and Baska Mask, the anesthesiologist opened the patientŌĆÖs mouth using the right thumb and index finger, held the bite block of the device with the left hand, and pushed it past the front teeth toward the hard palate, avoiding the tongue. Especially for the Baska Mask, the anesthesiologist used the extended hand-tab to control the flexion to help negotiate the palato-pharyngeal curve (Fig. 1A). The i-gel and Baska Mask were pushed until a definitive resistance was felt. At this point, the tip of the mask should be located at the upper esophageal opening.
All procedures were performed by a single anesthesiologist who had previously conducted similar studies with more than 30 insertions of the Baska Mask.
Effective ventilation was confirmed by EtCO2 waveforms and bilateral thoracic movements. In the case of a critical leak because of the absence of effective ventilation after inserting the device, the following manipulations were performed first: pushing and pulling of the device, neck extension and flexion, jaw thrust, and chin lift. If the proper airway was not achieved after these maneuvers, the device was removed and a device with a different size was re-inserted. Endotracheal intubation was performed immediately after insertion failure, which was defined as three or more attempted insertions. The insertion time was defined as the time until the first EtCO2 waveform appeared on the monitor after proper device insertion.
The OLP was measured before pneumoperitoneum and was determined by adjusting the expiratory valve of the breathing circle to 40 cmH2O (fixed fresh gas flow, 3 L/min) and recording the pressure when equilibrium was reached [12]. The OLP was defined as the pressure at which audible gas leakage was detected with a stethoscope at the throat site. The flexible fiber-optic scope (external diameter, 3.1 mm; Olympus Optical, Tokyo, Japan) was inserted into the device to observe laryngeal structures such as vocal cords. The fiber-optic view of the glottis was graded according to the following scoring system: 1, vocal cord only; 2, vocal cords plus posterior epiglottis visible; 3, vocal cords plus anterior epiglottis visible; 4, vocal cords not seen [13]. PAP and pulmonary compliance were measured and compared at T0, T1, T2, T3, T4, and T5 (T0, baseline; T1, 1 min after induction; T2, 5 min before CO2 pneumoperitoneum; T3, 5 min after start of CO2 pneumoperitoneum; T4, 5 min before removal of pneumoperitoneum; T5, 5 min after removal of pneumoperitoneum) using a spirometer from Primus Dr├żger anesthesia ventilator (Dr├żger Medical GmbH, Germany). The leak fraction was calculated using the following formula:
The device was removed when the patient began to respond to verbal commands. Emergence from general anesthesia was performed by an unblinded investigator who was not involved with this study. Additionally, complications, such as bloodstains on the device, teeth or lip injury, coughing, vomiting, and bronchospasm, were confirmed immediately after device removal. Desaturation was defined as less than 90% oxygen saturation on pulse oximetry. Gastric distention was defined as the requirement of a gastric drain tube insertion by the surgeon, due to the inflated stomach that interfered with surgical exposure. Aspiration was defined as hypoxia after removal of the device with signs of chest infiltrate in postoperative chest radiography. Coughing was defined as at least four episodes of coughs, each lasting for more than 2 s, after device removal. Bronchospasm was defined as desaturation and laryngeal stridor after device removal [14ŌĆō18].
In addition, the patients were assessed for sore throat, dysphonia, and dysphagia 1 h after the surgery. Sore throat was defined as complaints of throat discomfort on enquiry. Dysphonia was defined as hoarseness of voice noted by the patient. Dysphagia was defined as pain when swallowing saliva [19]. Data from these complications were collected by a blinded investigator.
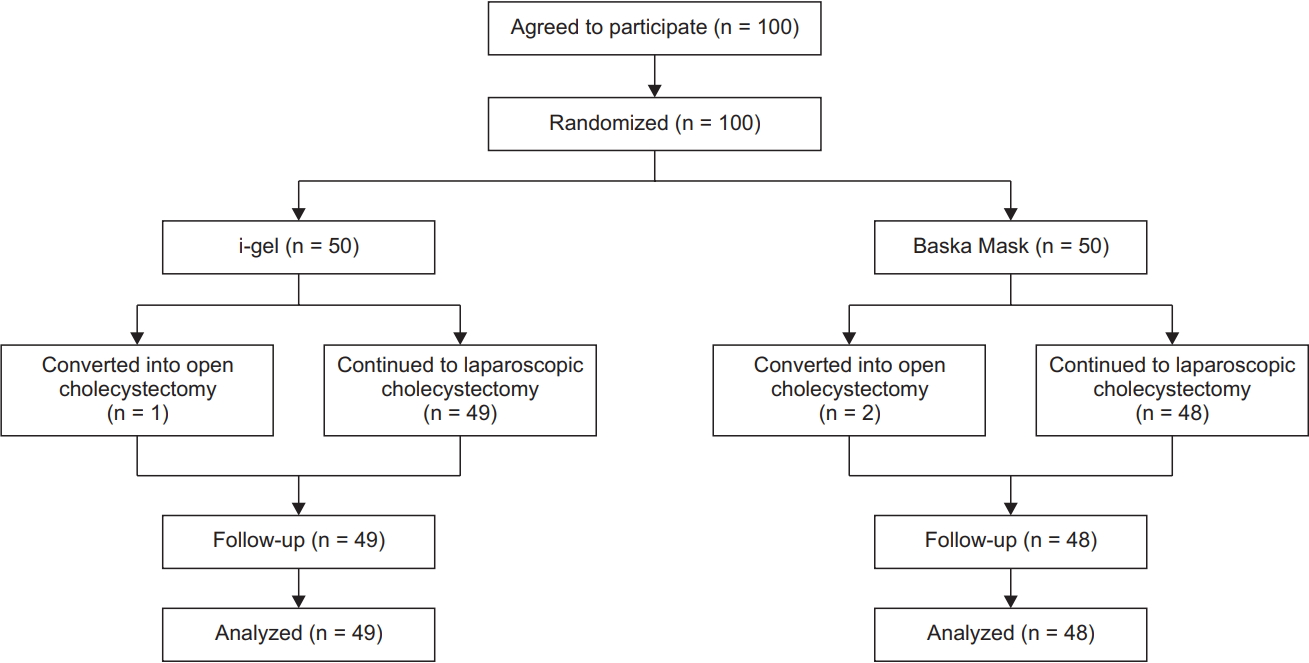
The sample size was calculated based on the data from a pilot study of 30 patients in the i-gel and Baska Mask groups (15 patients each), in which the OLP was measured as 26.1 ┬▒ 4.3 cmH2O and 29.3 ┬▒ 6.1 cmH2O, respectively. The sample size calculation using the above data at a two-tailed ╬▒ = 0.05 and 80% power, determined that 44 subjects were needed to detect statistically significant differences between the groups. Fifty patients per group were recruited to allow for potential dropouts. Using a computer-generated random number list, the 100 participants were randomly allocated to the i-gel group (n = 50) or Baska Mask group (n = 50).
Data, presented as mean ┬▒ standard deviation or number of patients (%), were recorded using a data collection sheet and analyzed using SPSS version 18 software (IBM Corp., USA). Continuous variables were analyzed using the StudentŌĆÖs t-test. Categorical data were analyzed using the chi-squared or FisherŌĆÖs exact test. A P value of < 0.05 was considered statistically significant.
In total, 50 patients each were assigned to the i-gel and Baska Mask groups. Three patients were excluded, one in the i-gel group and two in the Baska Mask group, because in them, laparoscopic cholecystectomy was converted to open cholecystectomy during surgery (Fig. 2). The patientsŌĆÖ characteristics and anesthetic data did not differ between the two groups (Table 1).
Table 2 summarizes the data regarding insertion in the i-gel and Baska Mask groups. Most of the devices were successfully inserted on the first attempt, except for one i-gel device, which was successfully inserted on the second attempt (P = 0.320). OLP was higher in the Baska Mask group (29.6 ┬▒ 6.8 cmH2O) than in the i-gel group (26.7 ┬▒ 4.5 cmH2O) (P = 0.014). There was no significant difference in the insertion time and fiber-optic view of the glottis between the two groups (P = 0.165 and P = 0.855, respectively). During pneumoperitoneum, an audible air leak developed in four patients in the i-gel group and three patients in the Baska Mask group (P = 0.512). Three patients in the i-gel group and six patients in the Baska Mask group required airway manipulations (P = 0.233).
There were no statistically significant differences between the two groups with regard to changes in the heart rate and mean arterial pressure at each measured time (i.e., T1, T2, T3, T4, and T5) (Fig. 3). There were no statistically significant differences between the two groups with regard to changes in PAP and lung compliance at each measured time (i.e., T1, T2, T3, T4, and T5) (Supplementary Fig. 1). Changes in leak fraction showed no statistically significant differences between the two groups (Supplementary Fig. 2).
The incidence of perioperative complications was small and not statistically significant. The incidences of sore throat, dysphonia, and dysphagia were not significantly different between the two groups (Table 3).
SAD offers an alternative airway to traditional tracheal intubation with potential benefits, including easy insertion and low laryngopharyngeal morbidity. However, it is more likely to leak than an endotracheal tube due to its structural characteristics. Thus, the OLP is a critical factor when deciding to use the SAD. OLP values that are higher than PAP values ensure airway maintenance without leakage. In general, intra-abdominal pressure is known to increase by an average of 15 mmHg during laparoscopic surgery [20]. As a result, PAP increases by approximately 50%, and lung compliance decreases by approximately 25% [21ŌĆō23]. Thus, laparoscopic surgeries cause more unfavorable ventilatory conditions than general operations with lower PAPs. In this regard, investigating the function of SADs during laparoscopic surgeries with higher PAPs, which cause the aforementioned disadvantages, could be appropriate. In conclusion, SAD with a higher OLP value than PAP may be recommended for laparoscopic surgery.
In this study, the OLP of the Baska Mask was 29.6 ┬▒ 6.8 cm-H2O, which was higher than that measured with the i-gel (26.7 ┬▒ 4.5 cmH2O). A previous study reported that inflatable SADs, such as LMA Supreme and LMA Proseal, have higher OLPs than that of the i-gel [24]. The cuff of the Baska Mask is connected to the central channel of the device. When the airway pressure increases during inspiration, the cuff inflates itself to ensure closer attachment to the surrounding surface. Therefore, the Baska Mask is considered to have a relatively high OLP, and it may be applicable in surgeries such as laparoscopic gynecology surgery, in which patients are in the Trendelenburg position, which can further increase PAP.
This study also showed that PAP increased and lung compliance decreased during pneumoperitoneum in both groups and that the changing pattern was similar between the two groups, with no statistically significant difference. In addition, the Baska Mask group also showed no statistically significant difference in leak fraction compared with the i-gel group. Lai et al. [4] reported that the i-gel group did not show a significant difference in leak fraction compared with the endotracheal tube. Although the OLP value of the Baska Mask group was not measured in the pneumoperitoneum, effective ventilation may be possible in laparoscopic surgery as an aforementioned result of the leak fraction value. Therefore, we believe that the Baska Mask can be an alternative in patients who can tolerate the use of the i-gel device during laparoscopic cholecystectomy.
One of the advantages of the SAD is that there is less hemodynamic instability when inserting the device compared with inserting the tracheal tube [25,26]. In this study, there was almost no difference in the heart rate and mean arterial pressure due to device insertion between the two groups. The changes in heart rate and mean arterial pressure between the two groups were similar, without a statistically significant difference, and the Baska Mask provided hemodynamic stability similar to that provided by i-gel.
In this study, the cuff size of the Baska Mask was wider than those of the i-gel. Circumferences of size 3 of i-gel and Baska Mask were 11.7 cm and 13.8 cm, and those of size 4 were 13 cm and 14.8 cm, respectively (Figs. 1B and 1C). In addition, Alexiev et al. [7] showed that the Baska Mask was more difficult to insert than the classical laryngeal mask. Therefore, difficulty in insertion was anticipated before this study. However, the ease of insertion, number of first insertion attempts, and insertion time, which reflect the difficulty of insertion were not significantly different between the two groups. We used the extended handtab of the Baska Mask to control the flexion to adjust the angle. Therefore, ease of insertion was possibly similar to that of i-gel. However, there are only few studies related to the Baska Mask [7,8]; hence, further studies are needed.
The Baska Mask is characterized by a relatively large cuff and the process of cuff inflation at inspiration and cuff deflation at expiration during anesthesia. For this reason, it is expected that frequent stimulation on surrounding tissues in the Baska Mask group would lead to a higher incidence of complications such as postoperative sore throat compared with that in the i-gel group. However, there was no statistically significant difference in the incidence of postoperative complications between the two groups. Similarly, a study comparing the Baska Mask and LMA Supreme reported that complications such as mucosal injury were more frequent with the LMA Supreme [8]. Additionally, Brimacombe et al. [27], who compared the face mask and LMA, reported that the incidence of complications, such as sore throat, increased as the LMA cuff volume increased, with statistically significantly higher number of complications occurring with the use of larger cuff volumes. Hence, complications such as sore throat are thought to be caused by the volume of air inflated into the cuff rather than the size of the cuff. The cuff of the Baska Mask used in this study is not artificially pressurized but is self-inflated; thus, the cuff does not become bulky. Therefore, it is thought that the Baska Mask is less likely to damage or stimulate surrounding tissues compared with i-gel.
This study has some limitations. First, OLP was not compared in the presence of pneumoperitoneum. When a maneuver was performed for the measurement of OLP in the presence of increased PAP during pneumoperitoneum, the patientŌĆÖs airway maintenance during surgery was likely to be difficult because of the deviation of the fitted device. For safety, there was a limitation in measuring the OLP in the presence of pneumoperitoneum. Second, this study involved device insertion and removal by an unblinded investigator. Hence, the possibility of bias could not be excluded.
In conclusion, compared to the i-gel, the Baska Mask had a higher OLP. Additionally, there were no differences in complications in the setting of laparoscopic cholecystectomy. Therefore, the Baska Mask can be used as an alternative device to the i-gel, and its use can be extended to surgical situations wherein PAP can be further increased through a higher OLP.
NOTES
Author Contributions
So Ron Choi (Investigation)
Tae Young Lee (Investigation; WritingŌĆōoriginal draft)
Sung Wan Kim (Data curation; Investigation)
Sang Yoong Park (Formal analysis)
Chan Jong Chung (Conceptualization; Supervision; WritingŌĆōreview & editing)
Jeong Ho Kim (Supervision; WritingŌĆōreview & editing)
Supplementary Materials
Futher detailes are presented in the online version of this article (Available from https://doi.org/10.4097/kja.19195).
Supplementary┬ĀFig.┬Ā1.
Changes of peak airway pressure (A) and lung compliance (B) between the I-gel group and Baska Mask group. Values are expressed as mean ┬▒ standard deviation. There were no significant differences in peak airway pressure and lung compliance between the groups. T1: 1 min after induction, T2: 5 min before CO2 pneumoperitoneum, T3: 5 min after start of CO2 pneumoperitoneum, T4: 5 min before removal of pneumoperitoneum, T5: 5 min after removal of pneumoperitoneum.
Supplementary┬ĀFig.┬Ā2.
Changes of leak fraction between the I-gel group and the Baska Mask group. Values are expressed as mean ┬▒ standard deviation. There were no significant differences in leak fraction between the groups. T1: 1 min after induction, T2 : 5 min before CO2 pneumoperitoneum, T3: 5 min after start of CO2 pneumoperitoneum, T4: 5 min before removal of pneumoperitoneum, T5: 5 min after removal of pneumoperitoneum.
Fig.┬Ā1.
Appearances of Baska Mask and i-gel. (A) Flexing the Baska Mask using the hand-tab. (B) Circumferences of size 3 of i-gel and Baska Mask were 11.7 cm and 13.8 cm, respectively. (C) Circumferences of size 4 of i-gel and Baska Mask were 13 cm and 14.8 cm, respectively.
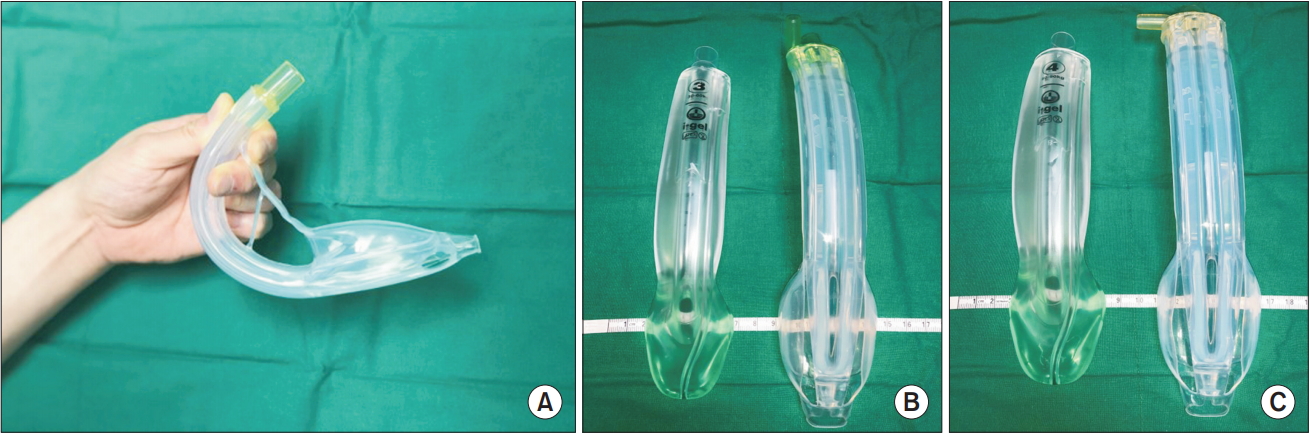
Fig.┬Ā3.
Changes in the heart rate (A) and mean arterial pressure (B) between the i-gel group and Baska Mask group. Values are presented as mean ┬▒ SD. There was no significant difference in the heart rate and mean arterial pressure between the groups. T0: baseline, T1: 1 min after induction, T2: 5 min before CO2 pneumoperitoneum, T3: 5 min after start of CO2 pneumoperitoneum, T4: 5 min before removal of pneumoperitoneum, T5: 5 min after removal of pneumoperitoneum.

Table┬Ā1.
PatientsŌĆÖ Characteristics and Anesthetic Data
| Variable | i-gel (n = 49) | Baska Mask (n = 48) | P value |
|---|---|---|---|
| Age (yr) | 52.4 ┬▒ 13.3 | 48.2 ┬▒ 11.0 | 0.095 |
| Sex (M/F) | 18/31 | 21/27 | 0.538 |
| ASA (1/2) | 14/35 | 20/28 | 0.206 |
| Height (cm) | 160.9 ┬▒ 8.0 | 163.7 ┬▒ 8.0 | 0.094 |
| Weight (kg) | 64.6 ┬▒ 11.4 | 62.7 ┬▒ 10.9 | 0.416 |
| Mallampati score (1/2/3/4) | 19/28/2/0 | 11/33/4/0 | 0.202 |
| Thyromental distance (cm) | 7.5 ┬▒ 1.0 | 7.8 ┬▒ 0.7 | 0.058 |
| Inter-incisor distance (cm) | 4.5 ┬▒ 0.7 | 4.8 ┬▒ 0.5 | 0.093 |
| Anesthetic time (min) | 58.1 ┬▒ 16.2 | 59.2 ┬▒ 11.8 | 0.723 |
| Pneumoperitoneum time (min) | 25.7 ┬▒ 14.4 | 21.4 ┬▒ 11.3 | 0.109 |
| Total propofol used (mg) | 396.1 ┬▒ 127.3 | 382.8 ┬▒ 95.5 | 0.565 |
| Total remifentanil used (╬╝g) | 381.67 ┬▒ 151.0 | 394.1 ┬▒ 133.3 | 0.671 |
| Analgesic method (0/1/2)* | 20/28/1 | 21/20/7 | 0.054 |
Table┬Ā2.
Insertion of i-gel and Baska Mask
| Complications | i-gel (n = 49) | Baska Mask (n = 48) | P value |
|---|---|---|---|
| Size (3/4) | 27/22 | 26/22 | 0.926 |
| Attempt no. (1/2) | 48/1 | 48/0 | 0.320 |
| Insert time (min) | 29.0 ┬▒ 10.3 | 31.4 ┬▒ 6.3 | 0.165 |
| Insert resistance (1/2/3/4)* | 42/7/0/0 | 44/4/0/0 | 0.355 |
| Fiberoptic view (1/2/3/4)ŌĆĀ | 42/5/2/0 | 41/4/3/0 | 0.855 |
| Manipulation frequency (0/1/2) | 46/3/0 | 42/6/0 | 0.233 |
| OLP (cmH2O) | 26.7 ┬▒ 4.5 | 29.6 ┬▒ 6.8 | 0.014 |
Table┬Ā3.
Perioperative Complications
References
1. Park SK, Ko G, Choi GJ, Ahn EJ, Kang H. Comparison between supraglottic airway devices and endotracheal tubes in patients undergoing laparoscopic surgery: A systematic review and meta-analysis. Medicine (Baltimore) 2016; 95: e4598.



2. Dhanda A, Singh S, Bhalotra AR, Chavali S. Clinical comparison of i-gel supraglottic airway device and cuffed endotracheal tube for pressure-controlled ventilation during routine surgical procedures. Turk J Anaesthesiol Reanim 2017; 45: 270-6.




3. Park SY, Rim JC, Kim H, Lee JH, Chung CJ. Comparison of i-gelŌōć and LMA SupremeŌōć during laparoscopic cholecystectomy. Korean J Anesthesiol 2015; 68: 455-61.




4. Lai CJ, Liu CM, Wu CY, Tsai FF, Tseng PH, Fan SZ. I-Gel is a suitable alternative to endotracheal tubes in the laparoscopic pneumoperitoneum and trendelenburg position. BMC Anesthesiol 2017; 17: 3.




5. Sharma B, Sehgal R, Sahai C, Sood J. PLMA vs. I-gel: a comparative evaluation of respiratory mechanics in laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol 2010; 26: 451-7.



6. Alexiev V, Salim A, Kevin LG, Laffey JG. An observational study of the BaskaŌōć mask: a novel supraglottic airway. Anaesthesia 2012; 67: 640-5.


7. Alexiev V, Ochana A, Abdelrahman D, Coyne J, McDonnell JG, O'Toole DP, et al. Comparison of the Baska(Ōōć) mask with the single-use laryngeal mask airway in low-risk female patients undergoing ambulatory surgery. Anaesthesia 2013; 68: 1026-32.


8. Foo LL, Shariffuddin II, Chaw SH, Lee PK, Lee CE, Chen YS, et al. Randomized comparison of the Baska FESS mask and the LMA Supreme in different head and neck positions. Expert Rev Med Devices 2018; 15: 597-603.


9. H├Ėymork SC, Raeder J, Grimsmo B, Steen PA. Bispectral index, predicted and measured drug levels of target-controlled infusions of remifentanil and propofol during laparoscopic cholecystectomy and emergence. Acta Anaesthesiol Scand 2000; 44: 1138-44.


10. Liu SY, Leighton T, Davis I, Klein S, Lippmann M, Bongard F. Prospective analysis of cardiopulmonary responses to laparoscopic cholecystectomy. J Laparoendosc Surg 1991; 1: 241-6.


11. Baska Mask and Baska FESS Mask sizes [Internet]. Baska Versatile Laryngeal Mask (BVLM) Pty Ltd (Australia) [cited 2019 Jun 5]. Available from https://baskamask.net/baska-mask-sizes/
12. Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth 1999; 82: 286-7.



13. Keller C, Brimacombe J, P├╝hringer F. A fibreoptic scoring system to assess the position of laryngeal mask airway devices. Interobserver variability and a comparison between the standard, flexible and intubating laryngeal mask airways. Anasthesiol Intensivmed Notfallmed Schmerzther 2000; 35: 692-4.


14. Lee YC, Yoon KS, Park SY, Choi SR, Chung CJ. A comparison of i-gelTM and Laryngeal Mask Airway SupremeTM during general anesthesia in infants. Korean J Anesthesiol 2018; 71: 37-42.



15. Maltby JR, Beriault MT, Watson NC, Fick GH. Gastric distension and ventilation during laparoscopic cholecystectomy: LMA-Classic vs. tracheal intubation. Can J Anaesth 2000; 47: 622-6.



16. Raghavendran K, Nemzek J, Napolitano LM, Knight PR. Aspiration-induced lung injury. Crit Care Med 2011; 39: 818-26.



17. Tung A, Fergusson NA, Ng N, Hu V, Dormuth C, Griesdale DG. Pharmacological methods for reducing coughing on emergence from elective surgery after general anesthesia with endotracheal intubation: protocol for a systematic review of common medications and network meta-analysis. Syst Rev 2019; 8: 32.




18. Jouan ZT, Jawan B, Lee JH. Pulmonary edema complicated by post-extubation laryngospasm: a case report. Changgeng Yi Xue Za Zhi 1997; 20: 309-12.

19. Budania LS, Chamala V, Rao M, Virmani S, Goyal KA, Nanda K. Effect of air, anesthetic gas mixture, saline, or 2% lignocaine used for tracheal tube cuff inflation on coughing and laryngotracheal morbidity after tracheal extubation. J Anaesthesiol Clin Pharmacol 2018; 34: 386-91.



20. Versichelen L, Serreyn R, Rolly G, Vanderkerckhove D. Physiopathologic changes during anesthesia administration for gynecologic laparoscopy. J Reprod Med 1984; 29: 697-700.

21. Pelosi P, Foti G, Cereda M, Vicardi P, Gattinoni L. Effects of carbon dioxide insufflation for laparoscopic cholecystectomy on the respiratory system. Anaesthesia 1996; 51: 744-9.


22. O'Malley C, Cunningham AJ. Physiologic changes during laparoscopy. Anesthesiol Clin North Am 2001; 19: 1-19.


23. Cunningham AJ, Brull SJ. Laparoscopic cholecystectomy: anesthetic implications. Anesth Analg 1993; 76: 1120-33.


24. Mukadder S, Zekine B, Erdogan KG, Ulku O, Muharrem U, Saim Y, et al. Comparison of the proseal, supreme, and i-gel SAD in gynecological laparoscopic surgeries. ScientificWorldJournal 2015; 2015: 634320.




25. Ismail SA, Bisher NA, Kandil HW, Mowafi HA, Atawia HA. Intraocular pressure and haemodynamic responses to insertion of the i-gel, laryngeal mask airway or endotracheal tube. Eur J Anaesthesiol 2011; 28: 443-8.