We present a case of a healthy man who developed a pulmonary embolism (PE) after arthroscopic shoulder surgery. He had an interscalene block (ISB) catheter inserted before the induction of general anesthesia and received a bolus of local anesthetic (LA). Interestingly, he developed dyspnea only on postoperative day (POD) 2, leading to the identification of an otherwise asymptomatic PE. It is important to exclude other causes of dyspnea in patients who have a low risk of developing symptomatic phrenic nerve block (PNB) before attributing dyspnea to the ISB; ISB has a secondary, albeit unintended, role of revealing asymptomatic lung pathologies. If the patient had not received ISB, his PE would have been missed and untreated, which could have led to an undesirable clinical outcome.
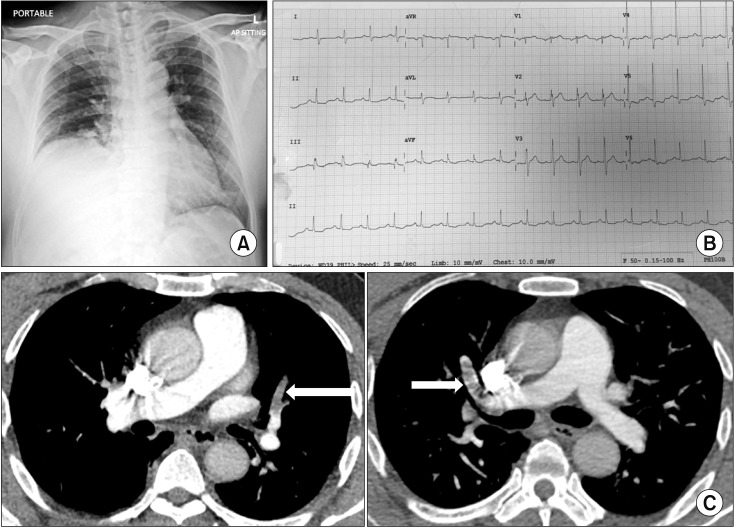
The patient gave permission for the case to be reported. He was a 57-year-old man, had American Society of Anesthesiologists physical status I, had a body mass index (BMI) of 28 kg/m2, was a non-smoker, and underwent right shoulder arthroscopic surgery for severe adhesive capsulitis under general anesthesia. A continuous ISB was performed before the induction of general anesthesia under ultrasound guidance using an in-plane approach. A bolus dose of 5 ml 1% lignocaine and 20 ml 0.5% bupivacaine was injected between the C5 and C6 roots within the interscalene groove (intra-fascial). The final position of the catheter tip was lateral to the interscalene groove (extra-fascial) due to technical difficulties. There were no immediate complications after the block, such as Horner's syndrome, hoarseness, or dyspnea. A perineural infusion was initiated with ropivacaine 0.2% at 5 ml/h post-operatively. On POD 2, the patient developed acute dyspnea when ambulating. His oxygen saturation was 70% in room air, which improved to 98% with 15 L/min oxygen delivered via a non-rebreathing face mask. The chest radiograph showed an elevated right hemidiaphragm (Fig. 1A). Ropivacaine infusion was stopped, the perineural catheter was removed, and the patient improved symptomatically. The cause of dyspnea was initially thought to be right PNB. However, a 12-lead electrocardiogram showed classic features of PE (Fig. 1B), and computed tomography pulmonary angiography revealed multiple segmental PEs (Fig. 1C). Doppler ultrasound of the lower limbs revealed a right soleal vein thrombosis. For this reason, the patient was started on anticoagulants and remained clinically well until discharge from the hospital on POD 9.
PNB resulting in ipsilateral hemidiaphragmatic paresis is a common side effect following ISB [1]. Most cases of PNB are transient and asymptomatic, particularly in healthy individuals. Even if PNB is symptomatic, it is mostly reported as mild dyspnea. In a prospective safety study of 1,505 patients who received continuous ISB after shoulder surgery, only 27% experienced mild dyspnea and none experienced severe dyspnea [2]. In general, PNB is well tolerated by healthy individuals without pulmonary pathology. This is explained by the ability to compensate for temporary diaphragmatic paralysis using the intercostal accessory muscles and increasing the expansion of the contralateral diaphragm. Thus, patients experience minimal decreases in tidal volume and pulmonary oxygen, leading to being clinically asymptomatic [3]. On the other hand, patients with high BMI or preexisting lung disease can experience shortness of breath and clinically significant hypoxemia, even with transient PNB.
As noted in a recent study [4] that examined diaphragm-sparing nerve blocks for shoulder surgery, ultrasound-guided ISB with small volumes (5 ml), dilute LA concentrations, and LA injection 4 mm lateral to the brachial plexus (extra-fascial) have been shown to reduce the risk of PNB; however, no single intervention can decrease its incidence below 20%. There have been several alternative diaphragm-sparing nerve blocks proposed for shoulder surgery, but their clinical efficacy requires further study. These are ultrasound-guided supraclavicular blocks with LA injection posterolateral to the brachial plexus, ultrasound-guided C7 root block, combined axillary-suprascapular nerve blocks, and the combined use of infraclavicular brachial plexus blocks and suprascapular nerve blocks.
In this case, the patient developed PE perioperatively. If he had not received an ISB and as a consequence had his respiratory mechanics had not been compromised with unilateral PNB, his PE could have gone undiagnosed; not all patients with PE are symptomatic. This diagnosis is supported by the fact that his symptoms resolved with the recovery of hemidiaphragmatic function after the PNB wore off. The index of suspicion for PE was never high, as the patient did not have any risk factors for venous thromboembolism (VTE) and VTE following shoulder arthroscopy surgery is reported to be rare, with an incidence of 0.15% [5].
In conclusion, ISB is the mainstay and gold standard for analgesia after shoulder surgery. PNB is a known side effect following ISB, but most cases are transient and asymptomatic, particularly in healthy individuals. We recommend diaphragm-sparing nerve blocks for shoulder surgery as an alternative for those at risk for symptomatic PNB. Nevertheless, anesthesiologists and surgeons should maintain a low threshold for ruling out other potential causes of acute dyspnea after an ISB before attributing it to the PNB that occurs with an ISB.