|
 |
|
|
Abstract
Arytenoid cartilage dislocation is not a common complication, but its delayed diagnosis reduces the therapeutic effect of treatment. A male patient underwent reversed total shoulder replacement surgery in the beach chair position under general anesthesia. The patient experienced postoperative hoarseness, and it was revealed that he had right arytenoid dislocation. Voice restoration was accomplished with closed reduction. We discussed changes in patient position during the operation and how they may contribute to the arytenoid dislocation. Flexion and a slight rotation of the neck during the operation can lead to an increase in intracuff pressure of the endotracheal tube. It is necessary to check neck position and monitor intracuff pressure in patients undergoing operations in the beach chair position. Also, the anesthesiologist should suspect arytenoid dislocation in the case of persistent hoarseness after surgery in the beach chair position.
Hoarseness is a common complication after tracheal intubation; its incidence is reported to be 14.4–50% [1,2]. Prolonged hoarseness after anesthesia is unusual, and its etiology is often difficult to establish. Prolonged hoarseness can be caused by pharyngeal and/or laryngeal trauma, which may induce hematoma and edema, injury to the recurrent or superior laryngeal nerves, and arytenoid cartilage dislocation [3,4]. Arytenoid cartilage dislocation is not a common complication after tracheal intubation; its incidence is less than 0.1% [5,6]. The signs and symptoms of such a dislocation are hoarseness, sore throat, painful swallowing, inspiratory stridor, cyanosis, and hypoxemia [7]. Traumatic and blind airway manipulation may be associated with arytenoid dislocation, but this complication also can be found after uneventful laryngoscopy and tracheal intubation [8,9].
We present a case of arytenoid dislocation caused by an uneventful tracheal intubation and extubation after arthroscopic shoulder surgery in the beach chair position.
A 65-year-old American Society of Anesthesiologists physical status classification II male (167 cm and 67 kg) was scheduled for a reversed total replacement of the right shoulder due to massive rotator cuff tear. He was diagnosed with hypertension and atrial fibrillation. He had been under general anesthesia twice before; once for a shoulder surgery and another time for a lumbar surgery. His physical and laboratory examinations were unremarkable.
Anesthesia was induced with thiopental 300 mg, rocuronium 50 mg, and remifentanil 30 µg intravenously. Complete muscle relaxation was confirmed before insertion of the endotracheal tube. Upon visualization of the larynx with direct laryngoscopy (Macintosh 3 laryngoscope blade), the glottis was classified as Cormack-Lehane Grade II. A 7.5-mm inner diameter endotracheal tube (Mallinckrodt TaperGuard™, Covidien, Tullamore, Ireland) without stylet was smoothly inserted into the trachea without difficulty on the first attempt and fixed at a depth of 22 cm. Anesthesia was maintained with oxygen, nitrous oxide, sevoflurane, and remifentanil (0.1–0.2 µg/kg/min). The operation was performed in the beach chair position, lasted 2 h 30 min, and was uneventful. The upper body was elevated 50 degrees in a neutral position. The head was turned to the left and flexed slightly to expose the surgical field. There was more than two fingerbreadths distance between the chin and the sternum. The head was fixed to the headrest with adhesive tape. The endotracheal tube was connected to the breathing circuit using a catheter mount. The breathing circuit was fixed with an elastic band to the headrest to avoid movement. During surgery, neither patient position nor the breathing circuit was disturbed.
After the operation, the endotracheal tube cuff was deflated and removed without any difficulty, severe coughing and vomiting did not occur. The patient did not complain of hoarseness in the postanesthesia care unit.
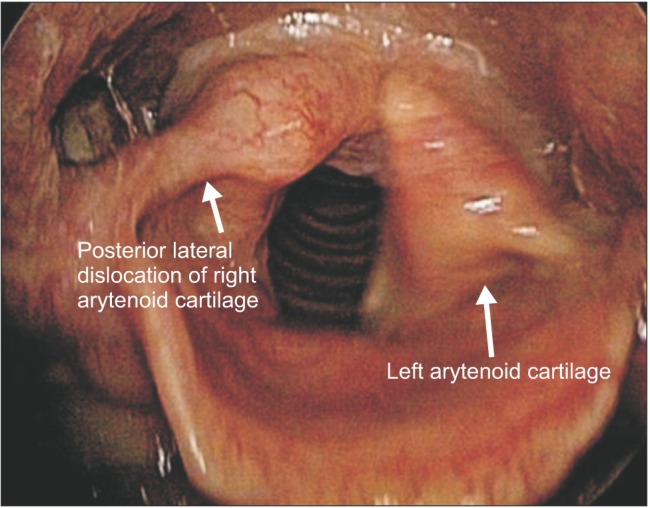
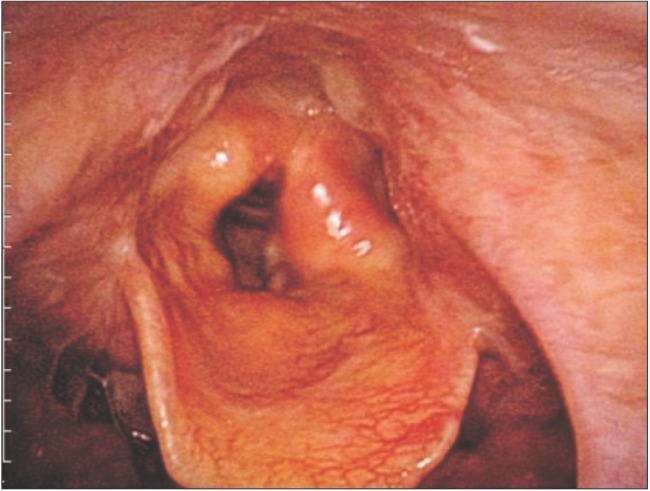
On postoperative day 1, the patient complained of hoarseness without other symptoms. The hoarseness persisted through postoperative day 4, when an ear, nose, and throat consult was done. An otorhinolaryngologist performed a fiber-optic laryngoscopy, which revealed a posterolateral dislocation of the right arytenoid cartilage (Figs. 1 and 2). On postoperative day 7, the hoarseness had not improved, so a closed reduction of the displaced cartilage was performed under general anesthesia. The patient was discharged from the hospital one day after the reduction without any improvement in his voice. In a routine follow-up two months later, the hoarseness was relieved; no recurrence of hoarseness has been reported since.
Hoarseness is a common postoperative complication, reported to have an incidence of up to 50%. Most cases are temporary, and the voice recovers within a few days without medical intervention. In only 0.8% of such cases, the hoarseness persists for > 1 week and does not spontaneously resolve [10]. Although arytenoid cartilage dislocation is related to tracheal intubation, it is a rare complication, occurring in only 0.023–0.1% of the cases requiring intubation [5,10]. It is one possible cause of prolonged hoarseness. An arytenoid dislocation is not life-threatening, but recovery becomes difficult if appropriate treatment is delayed. Early diagnosis and proper treatment are crucial for the optimal return of the voice. Arytenoid dislocation is easily misdiagnosed as vocal cord paralysis or paresis because the conditions have similar symptoms. Thus, it is important to remain aware of the possibility of arytenoid dislocation in cases of postoperative prolonged hoarseness [11].
The most common etiologic factor in arytenoid cartilage dislocation is intubation trauma, which is reportedly responsible for between 80 and 87% of cases, followed by external trauma, which accounts for 15% [4,11]. The remaining causes include insertion of laryngeal mask airway, transesophageal echocardiography probe, and gastroscopy. There are several noteworthy contributing factors and possible mechanism of arytenoid dislocation following intubation. During endotracheal intubation, posterolateral dislocation of the left arytenoid occurs more frequently. Most frequently, the tracheal tube is held in the right hand and the endoscope in the left, and this conformation allows the distal end of the endotracheal tube to apply direct pressure on the left arytenoid cartilage in the posterolateral direction [7]. Another possible mechanism is a posterosuperior dislocation of the arytenoid cartilage during extubation if the cuff of the endotracheal tube is not fully deflated [12]. Several cases of arytenoid dislocation have occurred in patients with systemic illness, such as renal failure or acromegaly. Wang [13] reported that significant force is necessary to disrupt the major support structure of the cricoarytenoid joint and produce subluxation in a normal larynx. Thus, weakness secondary to systemic illness may contribute to the occurrence of the dislocation. In our patient, there were no systemic illnesses known to be contributing factors.
In our patient, the cause of arytenoid cartilage dislocation was unclear, and a number of possible causes have been identified. There is a possibility of damage during tracheal intubation or extubation. Arytenoid dislocation associated with tracheal intubation is statistically the most common cause and more commonly occurs in the left arytenoid. In our case, the intubation was not traumatic and the dislocation was on the right side. Also, there is little likelihood of arytenoid dislocation related to the extubation. Arytenoid dislocation during extubation usually occurs in the posterosuperior direction when the cuff of the endotracheal tube is not fully deflated. We fully deflated the cuff before extubation and the direction of the dislocation was posterolateral in our patient. Although we cannot completely rule out that trauma during tracheal intubation or extubation caused the dislocation, it is more likely that changes in the patient's position during the operation contributed to the dislocation. The beach chair position is very commonly employed for upper limb procedures. However, stabilization of the patient's head can be problematic in this position. The possible causes of arytenoid dislocation during the operation in the beach chair position are as follows. First, changes in the patient's position from supine to upright or from upright to supine may have contributed to the dislocation by altering the forces exerted by the endotracheal tube on the larynx. Second, neck flexion and a slight rotation of the neck toward the opposite direction during the surgical procedure can lead to an increase in intracuff pressure [14,15]. Kako et al. [14] reported that variation in head and neck position may alter the shape and length of the trachea and the position of the cuff, thereby resulting in an alteration in intracuff pressure. A dramatic increase in intracuff pressure was noted with neck flexion in their study. We did not measure intracuff pressure after intubation. If we had measured intracuff pressure, it would most likely have been possible to elucidate the cause of arytenoid dislocation in this case.
In summary, arytenoid cartilage dislocation associated with tracheal intubation is a rare complication, but recovery is difficult if appropriate treatment is delayed. Thus, early diagnosis and proper treatment is essential. It is necessary to pay attention to neck position and check intracuff pressure in patients who undergo operations in the beach chair position. Also, it is important that the anesthesiologist suspect arytenoid dislocation in cases of persistent hoarseness after surgery in the beach chair position.
References
1. Mencke T, Echternach M, Kleinschmidt S, Lux P, Barth V, Plinkert PK, et al. Laryngeal morbidity and quality of tracheal intubation: a randomized controlled trial. Anesthesiology 2003; 98: 1049-1056. PMID: 12717124.


2. Maruyama K, Sakai H, Miyazawa H, Toda N, Iinuma Y, Mochizuki N, et al. Sore throat and hoarseness after total intravenous anaesthesia. Br J Anaesth 2004; 92: 541-543. PMID: 14766717.



3. Rosenberg MK, Rontal E, Rontal M, Lebenbom-Mansour M. Arytenoid cartilage dislocation caused by a laryngeal mask airway treated with chemical splinting. Anesth Analg 1996; 83: 1335-1336. PMID: 8942611.


4. Rubin AD, Hawkshaw MJ, Moyer CA, Dean CM, Sataloff RT. Arytenoid cartilage dislocation: a 20-year experience. J Voice 2005; 19: 687-701. PMID: 16301111.


5. Szigeti CL, Baeuerle JJ, Mongan PD. Arytenoid dislocation with lighted stylet intubation: case report and retrospective review. Anesth Analg 1994; 78: 185-186. PMID: 8267162.


6. Kambic V, Radsel Z. Intubation lesions of the larynx. Br J Anaesth 1978; 50: 587-590. PMID: 666934.


8. Frink EJ, Pattison BD. Posterior arytenoid dislocation following uneventful endotracheal intubation and anesthesia. Anesthesiology 1989; 70: 358-360. PMID: 2913871.


9. Senoglu N, Oksuz H, Ugur N, Dogan Z, Kahraman A. Arytenoid dislocation related to an uneventful endotracheal intubation: a case report. Cases J 2008; 1: 251PMID: 18937836.



10. Yamanaka H, Hayashi Y, Watanabe Y, Uematu H, Mashimo T. Prolonged hoarseness and arytenoid cartilage dislocation after tracheal intubation. Br J Anaesth 2009; 103: 452-455. PMID: 19556269.



11. Sataloff RT, Bough ID Jr, Spiegel JR. Arytenoid dislocation: diagnosis and treatment. Laryngoscope 1994; 104: 1353-1361. PMID: 7968164.


12. Dudley JP, Mancuso AA, Fonkalsrud EW. Arytenoid dislocation and computed tomography. Arch Otolaryngol 1984; 110: 483-484. PMID: 6732593.


13. Wang RC. Three-dimensional analysis of cricoarytenoid joint motion. Laryngoscope 1998; 108: 1-17. PMID: 9546282.

14. Kako H, Krishna SG, Ramesh AS, Merz MN, Elmaraghy C, Grischkan J, et al. The relationship between head and neck position and endotracheal tube intracuff pressure in the pediatric population. Paediatr Anaesth 2014; 24: 316-321. PMID: 24238105.


15. Brimacombe J, Keller C, Giampalmo M, Sparr HJ, Berry A. Direct measurement of mucosal pressures exerted by cuff and non-cuff portions of tracheal tubes with different cuff volumes and head and neck positions. Br J Anaesth 1999; 82: 708-711. PMID: 10536547.