|
 |
|
|
Abstract
Thrombus-in-transit appears to increase the risk of mortality compared to pulmonary embolism alone and can require alteration in therapeutic plan. We present the case of a biatrial thromboembolus caught in transit across a patent foramen ovale diagnosed by intraoperative transesophageal echocardiogram in a 69-year-old female with acute pulmonary embolism and subsequent acute cerebral infarction. We suggest that echocardiography should be performed in a patient with suspected pulmonary thromboembolism to evaluate right heart function and diagnose emboli in transit.
Mobile, right-sided cardiac thrombi are reported in up to 20% of patients with pulmonary embolism [1] and increase mortality [2]. The presence of a patent foramen ovale (PFO) and pulmonary hypertension related to the pulmonary embolism may provoke paradoxical embolism, such as a stroke [3]. We present the case of a biatrial thromboembolus caught in transit across a PFO diagnosed by intraoperative transesophageal echocardiography in a 69-year-old female with acute pulmonary embolism and subsequent acute cerebral infarction.
A 69-year-old female patient who had a history of asthma was transferred to our hospital for the surgical treatment of pulmonary embolism. She did not have any previous deep vein thrombosis or pulmonary embolism and was not diagnosed with any malignancy. She was admitted to private clinic with dyspnea at rest for 10 days. On the next day of admission to private clinic, her oxygen saturation was decreased to 60%. Intubation was done and pulmonary thromboembolism was diagnosed by chest computed tomogram (Fig. 1).
Upon arrival at the emergency department of our hospital, she had tachycardia of 131 beats/min and blood pressure of 166/95 mmHg. Mental status was drowsy with midazolam infusion and neurologic deficits could not be assessed due to sedation. Initial ECG showed sinus tachycardia with right bundle branch block. Initial laboratory test showed high serum level of D-dimer. Others were unremarkable.
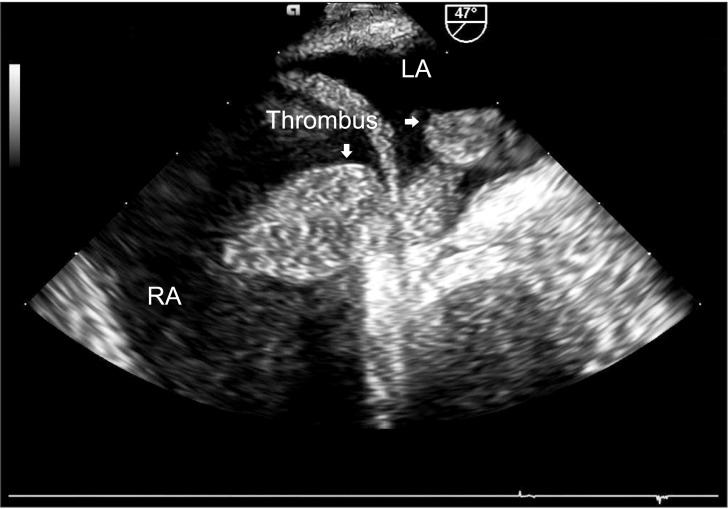
On arrival at the operating room, blood pressure (BP) was 78/42 mmHg, and pulse rate was 137 beats/min without any inotropic support. Pulse oximetry showed 93% saturation while breathing 100% oxygen. Cerebral oximetry showed 73% and 67% saturation on the left and right sides, respectively. Initial arterial blood gas analysis (ABG) showed pH of 7.097, partial pressure of carbon dioxide (PaCO2) of 76 mmHg, partial pressure of oxygen (PaO2) of 140 mmHg, and bicarbonate of 23.8 mmol/L with 1.0 fractional inspired oxygen concentration (FIO2). Pulmonary artery catheter was not inserted. After induction of anesthesia, transesophageal echocardiogram showed a dysfunctional and dilated right ventricle and a large serpentine, mobile mass in the right atrium and extending to the left atrium through a PFO (Fig. 2). Under hypothermic cardiopulmonary bypass (CPB) with rectal temperature 28℃, fresh thromboemboli in bilateral pulmonary arteries and both atria were removed, and PFO was closed (Fig. 3). The value of cerebral oximetry was decreased within the 30% change of the baseline value and recovered to the baseline value after the weaning of CPB. The patient's ABG after weaning from CPB showed pH of 7.365, PaCO2 of 32 mmHg, and PaO2 of 327 mmHg at FIO2 of 1.0. She was hemodynamically stable (systemic BP; 97/57 mmHg, central venous pressure; 13 mmHg) and transferred to intensive care uint (ICU) with the infusion of vasopressin, norepinephrine, isosorbide dinitrate, and milrinone.
Immediately after admitted to ICU, she could open her eyes to verbal stimuli and move her extremities. She developed right-sided hemiplegia eight hours after the surgery. Brain MRI revealed acute infarction in the territory supplied by the left middle cerebral artery and multifocal, embolic infarctions scattered throughout the right cerebrum. At one day after surgical embolectomy, she underwent an urgent decompressive craniectomy. However, right hemiplegia was not improved and her mental status was drowsy after surgery. Six months later, she was transferred to another hospital for the conservative treatment including long-term ventilatory support without improvement of neurologic deficits.
Right heart thrombi are referred to as "emboli-in-transit" since they represent mobilized thrombi that are lodged temporarily in the right atrium or ventricle. This situation is rare but life threatening [2]. The prevalence of emboli-in-transit in patients with pulmonary embolism ranges from 4 to 20% [1,4] and may be underestimated due to lack of routine echocardiography.
Foramen ovale is a remnant from the fetal circulation which acts like a door capable of opening from the right to the left side. In contrast to the atrial septal defect, the patent foramen ovale is not a permanent defect [5]. Patent foramen ovale is found in up to 27% of normal adults [6]. Despite high prevalence rate of PFO, paradoxical embolism does not occur ordinarily The clinical diagnosis of paradoxical embolism is almost always presumptive and is suspected in patients who have a venous thrombus, a right-to-left shunt and evidence of arterial embolism [7]. In patients with pulmonary embolism, PFO is an independent predictor of mortality (odds ratio, 11.4) and increases the incidence of ischemic stroke [3].
The treatment of choice for emboli-in-transit is controversial. In a recent review, surgical thromboembolectomy in patients with a thromboembolus caught in transit across a PFO showed a trend toward improved survival and significantly reduced systemic emboli compared to anticoagulation [6], although mortality after pulmonary embolectomy has been reported as 27-41% [8,9]. Thrombolysis in these patients may cause fragmentation of thrombus and systemic embolization, resulting in increased mortality [4,10].
Computed tomogram is considered as gold standard to confirm the diagnosis of pulmonary embolism [11]. However, transesophageal echocardiography is non-invasive and useful for the differentail diagnosis including acute valvular dysfuntion, aortic dissection, or tamponade. Bed-side echocardiography is useful, when computed tomogram is not available due to hemodynamic instbility. In addiiton, intraoperative echocardiograpy enables the diagnosis of emboli-in-transit, which in turn prevents the use of thrombolytic treatment and its complicaitons.
Considering the increased mortality and required alteration in therapeutic plan associated with PFO in patients with pulmonary embolism, early echocardiography may identify impending paradoxical emboli and make the prompt decision for the treatment. Also, serial echocardiography may give important information during follow-up by evaluating the response to treatment. We suggest that echocardiography should be performed in a patient with suspected pulmonary thromboembolism who is in critical condition to evaluate right heart function and diagnose pulmonary emboli in transit.
References
1. Casazza F, Bongarzoni A, Centonze F, Morpurgo M. Prevalence and prognostic significance of right-sided cardiac mobile thrombi in acute massive pulmonary embolism. Am J Cardiol 1997; 79: 1433-1435. PMID: 9165180.


2. Mollazadeh R, Ostovan MA, Abdi Ardekani AR. Right cardiac thrombus in transit among patients with pulmonary thromboemboli. Clin Cardiol 2009; 32: E27-E31. PMID: 19330852.

3. Konstantinides S, Geibel A, Kasper W, Olschewski M, Blümel L, Just H. Patent foramen ovale is an important predictor of adverse outcome in patients with major pulmonary embolism. Circulation 1998; 97: 1946-1951. PMID: 9609088.


4. Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest 2002; 121: 806-814. PMID: 11888964.


5. Scheuerle A. Clinical differentiation of patent foramen ovale and secundum atrial septal defect: a survey of pediatric cardiologists in Dallas, Texas, USA. J Registry Manag 2011; 38: 4-8. PMID: 22097699.

6. Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc 1984; 59: 17-20. PMID: 6694427.


7. Ali Kausar Rushdi Y, Hina H, Patel B, Cross FW. The incidence of peripheral arterial embolism in association with a patent foramen ovale (right-to-left shunt). JRSM Short Rep 2011; 2: 35PMID: 21637396.


8. Fauveau E, Cohen A, Bonnet N, Gacem K, Lardoux H. Surgical or medical treatment for thrombus straddling the patent foramen ovale: impending paradoxical embolism? Report of four clinical cases and literature review. Arch Cardiovasc Dis 2008; 101: 637-644. PMID: 19056070.


9. Kilic A, Shah AS, Conte JV, Yuh DD. Nationwide outcomes of surgical embolectomy for acute pulmonary embolism. J Thorac Cardiovasc Surg 2013; 145: 373-377. PMID: 22341655.


10. Myers PO, Bounameaux H, Panos A, Lerch R, Kalangos A. Impending paradoxical embolism: systematic review of prognostic factors and treatment. Chest 2010; 137: 164-170. PMID: 19592472.


11. Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P, et al. Guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 2008; 29: 2276-2315. PMID: 18757870.


- TOOLS