Bradycardia during laparoscopic surgery due to high flow rate of CO2 insufflation
Article information
Pneumoperitoneum, using carbon dioxide (CO2), is used to assist laparoscopic surgery by making distension of abdominal cavity and splitting up its content, which improves visualization. However, artificial pneumoperitoneum may cause complications, such as bradycardia and even cardiac arrest, which are originated from increased abdominal pressure and CO2 retention [1]. We experienced severe bradycardia after CO2 insufflation with high flow rate during laparoscopic gynecological surgery.
A 59-year-old woman (154 cm and 56 kg), without any remarkable past history except well controlled hypertension, has come to take a laparoscopic colpopexy. Midazolam 2.5 mg was administered intramuscularly, 30 minutes before she transferred to the operation room. On arrival, initial blood pressure (BP) and heart rate (HR) were 120/90 mmHg and 65 beats per minute (bpm), respectively, and peripheral oxygen saturation (SpO2) was 98%. Propofol 120 mg and rocuronium 40 mg were injected for induction. Intubation was done with 7.0 mm endotracheal tube, and tidal volume (9 ml/kg) and respiratory rate were regulated to maintain a normal end-tidal CO2 (ETCO2). Anesthesia was maintained with 50% oxygen and sevoflurane 2 vol% and remifentanil was administered as a 0.05 µg/kg/min infusion, simultaneously. ETCO2 was maintained about 35 mmHg and peak inspiratory pressure (PIP) was 15 cmH2O. Trocar (SAFE PASS TROCARR, Vaxcon co., Incheon, Korea), size of 11 mm, was inserted to 1 cm below the umbilicus to induce pneumoperitoneum. CO2 insufflation was started with an insufflator (Insufflator ML-GX, MGB Endoscope Co. Ltd, Seoul, Korea), and then her BP and HR suddenly decreased to 80/60 mmHg and 42 bpm, respectively. PIP has increased to 20 cmH2O, but ETCO2 and SpO2 did not change. It was thought to be a consequence of peritoneal stretching, owing to pneumoperitoneum, so CO2 insufflation was seized. Remifentanil infusion was stopped and atropine 0.5 mg was injected. Then, BP and HR became 120/80 mmHg and 60 bpm, respectively. CO2 insufflation was started again, but bradycardia and hypotension developed yet again, and BP and HR decreased to 62/32 mmHg and 23 bpm, respectively. Pressure limit of insufflator kept 12 cmH2O during CO2 insufflation, but we found the flow rate of CO2 insufflation was too high (20 L/min). Her vital signs became stabilized again after stopping insufflator and hyperventilation with 100% O2. Flow rate was adjusted to start as 1 L/min and increased to 3 L/min after 2 minutes. While adequate pneumoperitoneum was achieved, vital signs were stable without hypotension or bradycardia. There were no sudden bradycardia or hypotension during surgery and she was transferred to the recovery room without any hazardous event.
It is well known that laparoscopic surgery, using CO2 to make a pneumoperitoneum, has risks of pathophysiological cardiovascular changes, such as severe bradycardia, arrhythmia, and cardiac arrest requiring cardiopulmonary resuscitation [1]. Causes of such alteration are known to be associated with vagal-mediated cardiovascular reflex initiated by rapid peritoneum distension due to insufflation or gas embolism [2]. Limiting of intra-abdominal pressure (IAP) below 12-15 mmHg during insufflation is known to be effective to prevent pathophysiological changes of pneumoperitoneum [1].
Even though pressure limitations of insufflator were 12 mmHg in our cases, severe bradycardia has developed after insufflation. Gas embolism was ruled out because there were no changes in ETCO2 and SpO2 [1]. Arrhythmias developed after rapid stretching of peritoneum are transient and well respond to reduction of IAP [2], and our patients had recovered soon after stopping insufflations and hyperventilation with 100% O2; thus, we concluded the arrhythmias are a consequence of peritoneal distension due to rapid increase of IAP after CO2 insufflation with high flow rate. But, it was a question that how high flow rate of insufflator could affect the IAP in the circumstances of maintaining acceptable pressure limit.
We thought the system of insufflators was the clue. Jacobs et al. has reported the insufflations performance and patient safety during laparoscopy [3]. Insufflator works effectively when balance of pressure, resistance and flow in system is established. Accordingly, gas flow from insufflator patient's abdomen follows the Hagen-Poiseuille's law theoretically [3]:
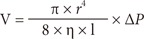
where V = gas flow, π = factor Pi, r = radius, 8 = constant, η = viscosity, l = length, and ΔP = pressure difference.
As the Hagen-Poiseuille's law states, gas flow rises in proportion to a rise in pressure, and depends on the smallest diameter of the system [3,4]. Thus, pressure will rise to keep a high flow rate when gas passes through high resistance channel of trocar, such as luer lock connector. Consequently, IAP will rise quickly to keep up the velocity if insufflator is regulated to keep a high flow rate as 20 L/min from the start of pneumoperitoneum. And more, insufflator that supports high flow rate usually uses over-pressure insufflation principle, which puts pressure much greater than preset value when starting insufflation [3]. Over-pressure system supply pressure beyond the preset value when starting of pneumoperitoneum and pressure decreased during insufflation break intermittently, until IAP reaches to the nominal pressure that has usually been preset to 12 mmHg [3,4]. As such, even if the preset value is limited to 12 mmHg, peak pressure of IAP will exceed the limit in an instant to keep up the fixed flow rate. Such repetitive exceeded IAP may stretch the peritoneum and stimulate vegal responses.
Cho and Min [1] had reported a similar case of severe bradycardia, which the flow rate was 50 L/min when the recommended flow rate was 1 L/min. Dhoste et al. [5] has reported that gradual abdominal insufflation to 12 mmHg with a slow flow rate of 1 L/min was associated with cardiovascular stability in elderly ASA III patients. We also experienced hemodynamic stability when using a gradual increase of flow rate from 1 L/min. So, we consider it is an appropriate start from the low flow rate as 1L/min in the beginning of pneumoperitoneum.
In conclusion, insufflation with high flow rate when establishing artificial pneumoperitoneum may increase IAP instantaneously and unexpected cardiovascular changes, such as hypotension, bradyarrhythmia or cardiac arrest, may occur. Therefore, not only maintaining IAP below 12-15 mmHg, but also keeping slow insufflation when establishing pneumoperitoneum is important and essential.