|
 |
|
|
Abstract
Many medical schools and hospitals throughout the world are equipped with a simulation center for the purpose of training anesthesiologists to perform both technical and non-technical skills. Because induction, maintenance, and emergence of general anesthesia are critical to patient welfare, various simulation mannequins and tools are utilized for the purpose of training anesthesiologists for safer patient care. Traditionally, anesthesia residency training mostly consisted of didactic lectures and observations. After completion of "traditional" training, anesthesia residents were allowed to perform procedures on patients under supervision. However, simulation would be a more effective training tool for which to teach anesthesiologists the skills necessary to perform invasive procedures, such as endotracheal intubation, central venous catheter insertion, and epidural catheter insertion. Recently, non-technical skills, such as the Anesthesia Non-Technical Skills developed by anesthesiologists from Aberdeen University, have been emphasized as an important training resource. Technical skills and non-technical skills can be learned by anesthesiology residents through a standardized and organized simulation program. Such programs would be beneficial in training anesthesia residents to work efficiently as a team in the operation room.
Anesthesiologists have played a key role in development of mannequin simulators and contributed to the development of simulation programs for education, training and research [1]. The first computer controlled mannequin simulator was SimOne® manufactured by Denson and Abrahamson in 1960s [2], but it was too large and expensive to apply to medical education. In 1968, Gordon developed Harvey®, a high-technology cardiopulmonary simulator [3]. Harvey has been used by medical students, nurses, residents and attending physicians. Harvey is capable of simulating auscultation sounds, blood pressure, arterial pulses, precordial impulses, normal heart sounds and murmurs. Most medical students were able to demonstrate high objective structured clinical examination (OSCE) scores after training with the Harvey® simulator [4]. An anesthetic drug physiology and pharmacology based computer simulation model, called Gasman®, was also developed. It was capable of showing anesthetic gas uptake, distribution and elimination [5]. In the 1980s, high fidelity mannequin simulators emerged in clinical anesthesia training (Comprehensive Anesthesia Simulation Environment [CASE] 1.2) for the purpose of teaching Anesthesia Crisis Resource Management (ACRM). Many skill trainers for various procedures training such as epidural catheter insertion, central venous catheter insertion and fiberoptic bronchoscopy were also developed during this period [6].
Such trials and discoveries were introduced to academic societies. International Meeting for Anesthesiology Societies provides many lectures and workshops on simulation. The Society for Simulation in Healthcare, an organization consisting of multi-disciplines in healthcare, has been organizing the annual International Meeting on Simulation for Healthcare every January since 2004, and has been publishing the official journal, "Simulation in Healthcare", every other month since 2006.
High fidelity simulators have been widely used for training anesthesiology residents and medical students since the 1990's. Anesthesiology residents trained with simulators responded more quickly, performed better and deviated less from the accepted procedure [7]. Technical performance and behaviors rated with simulation videotapes were also useful in assessing clinical competency [8]. HPS® simulator manufactured by Medical Education Technologies Inc. (METI) was used as an effective teaching tool for airway management, ventilator care and hemodynamic management in critical care medicine [9]. Issenberg et al. [10] reviewed 109 studies on high fidelity simulation learning, and providing feedback (47%), repetitive practice (39%), curriculum integration (25%), range of difficulty level (14%), multiple learning strategies (10%), capture clinical variation (10%), individualized learning (9%), defined outcomes (6%) and simulator validity (3%) were suggested as features and uses of high-fidelity medical simulators that lead to effective learning. Cook et al. [11] analyzed 609 articles from 10,903, and searched evidence of the effect of simulation on health profession education. It was suggested that technology-enhanced simulation training in health professions education is consistently associated with significant effects on the outcomes of knowledge, skills, and behaviors and with moderate effects on patient-related outcomes compared to no intervention.
The aim of this review was to introduce the necessities of simulation based training and education in the field of anesthesiology.
Simulation is a technique to replace or amplify real-patient experiences with guided experiences [12]. Various types of simulators are used to train and assess different levels of learners. These include mannequin simulators, human cadaver or animal models, computer-based simulation, haptic and/or virtual simulation, as well as simulation using standardized patients. Simulation has been an accepted part of training, assessment and research in high-reliability organizations, such as aviation, nuclear power, and military. Healthcare has adopted simulation from these fields for the purpose of training healthcare providers. Simulation-based learning has been used to shorten the gap that exists between the learning environment and the real clinical environment. Many skill trainers have been developed to actualize real clinical site especially for novice anesthesiologists [13].
Utilization of simulatiors has many advantages for medical education [14-18]: 1) learning can be focused on the level of trainees with various levels of difficulties; 2) learners can either learn the whole procedure process or just focus on certain tasks of the procedure; 3) learners have the opportunity to repetitively practice in quick succession; 4) learners learn in a safe environment where they can be allowed to learn from their mistakes rather than be rescued by their supervisor to keep the patient safe; 5) simulators can provide objective evidence of performance, offering potential for their use for assessment, both formative and summative; 6) simulation can provide practice on certain procedures such as cricothyrotomy, which is a critical life-saving procedure that is uncommon and rarely performed by anesthesiology residents.
However, simulation also comes with some limitations, especially when using high-technology simulators. Its high cost and the need for dedicated simulation rooms with audio-video system, separate debriefing rooms, simulation programs, trained faculty and staff are some of the barriers. Various simulation programs are needed, because limited experience of simulation can guide heuristic approach based on their own experiences [19].
There has been a growing trend for reduced medical training hours and decreased trainee exposure to clinical experience. This has led a question of whether there would be enough time for skills to be adequately learned through current training programs [20]. In addition to the trend of reduced training hours and clinical exposure, medical simulation has gained importance in medical education, because there is a perceived need for greater accountability to the public health and an increasing emphasis on patient safety [21]. Therefore, medical education should follow the trend of outcome based, competency based, and individual learning to achieve these goals.
Many of the skills required in anesthesia practice should be acquired by exercises and experiences rather than traditional lectures. Therefore, OSCE, problem-oriented learning (PBL) and clinical performance examination (CPX) were proposed as anesthesia education methods. Medical simulation has grown significantly world-wide in medical education, and simulation-based medical education is now a very important part of anesthesia training programs [22].
Training with high-fidelity simulators helps learners to adhere better to the American Society of Anesthesiologists (ASA) Difficult Airway Management guideline [23]. Other researchers reported better cardiopulmonary resuscitation performance after simulation [24], reduction in costs and complications related to central catheter insertion by simulation training [25], higher scores in cardiopulmonary bypass weaning after simulation based learning [26] and superior non-technical skills in simulation training groups. Simulation programs in anesthesia consists of, but not limited to, difficult airway management, lung separation, central venous catheter insertion, epidural block, hemodynamic monitoring, and so on [27-29].
Another application of medical simulation in anesthesia education is the assessment of skills and competency. Providing the opportunity to assess clinical performance in a scheduled, structured and standardized setting in conjunction with simulation based assessment may have the potential to be a valuable addition to the existing theoretical examination protocols in residency training [30]. For example, cannot intubate, cannot ventilate (CICV) scenario was used for anesthesiologist assessment [23]. Trainees showed improvement in the second CICV scenario by debriefing them about airway management algorithms. Situational stress, low familiarity with tracheal intubation instruments other than direct laryngoscopy and the lack of adherence to airway management algorithms are considered to be important causes for low scores. Although simulation training is demonstrated to be of value in the acquisition of skills, its effect diminishes in the long run and showed no difference in performance of central venous catheter insertion between clinically trained residents and residents with additional simulation training. Therefore, simulation acquired skills should be maintained by repetitive practice, constructive feedback and concrete assessment [17].
In anesthesiology, simulation research has fewer limitations with regard to ethical aspects than basic or clinical research. Simulation research has focused on the development of high fidelity simulators, the educational effects of combination of simulators, validity of educational tools such as global rating scale, application methods and so on.
Simulation is usually performed in specially designed simulation centers (Fig. 1), but, can be performed in real working areas. Stimulation in the real-world is called in situ simulation. In situ simulation has some advantages, for example, trainees are familiar with the equipment and environment, can cooperate with their own team, and no need for additional space.
Simulation programs should be designed according to the learning objectives and educational curriculum. Trainees as well as trainers should be familiar with learning objectives. The designing process is as follows: 1) review the process required to perform a procedure; 2) establish the steps required to perform a procedure; 3) develop a consensus on the sequence of the steps; 4) identify major performance milestones required to perform a procedure; 5) assure that trainees acquire the skills required for each step prior to advancing; 6) define the common as well as serious failure modes; and 7) design strategies that reduce the frequency of these errors [31].
Scenarios should be designed according to the entire simulation program. The designing process for scenarios are: 1) the scenario must include an opportunity for trainees to use judgments relevant to the training goals; 2) the scenario must have high fidelity for the clinical environment; 3) the scenario must include essential diagnostic and treatment skills required to manage the simulated condition; 4) practice experts must agree on these essential diagnostic and treatment skills; 5) an approach to evaluate, score and offer objective feedback must be provided following the scenario; 6) the scenario needs a copious, easy and clear description; 7) the scenario must include required skills embedded into the curriculum; and 8) crisis events are included in the compressed timeline.
After simulation with a simulator, debriefing is followed. It is well known that debriefing was first used to describe the account individuals gave on returning from a mission in the military. Debriefing on an event or activity and subsequent analysis is essential in the process of learning. However, not everyone is naturally capable of analyzing, understanding and assimilating learning experiences on their own, particularly those included in highly dynamic team based activities. The attempt to bridge this natural gap between experiencing an event and making sense of it has led to the evolution of the concept of post-experience analysis called debriefing. Elements of good debrief are the use of open ended questions, positive reinforcement, the use of cognitive aids, and good use of audiovisual capabilities [32]. Debriefing is performed according to the following process [33]: 1) identifying the impact of the experience; 2) identifying and considering the developed processes; 3) clarifying the facts, concepts, and principles; 4) identifying the ways in which emotion was involved; and 5) identifying different views formed by participants.
Assessment is a very important process in simulation training. Comprehensive checklists and global rating scales are frequently used. A greater level of involvement of simulation allows for more reliable assessment. A single prolonged and complicated scenario may offer more opportunities to demonstrate skills and non-technical skills, but scoring and assessment of the trainee is often challenging. Decreased working hours during the training course, increased focus on patient safety and greater accountability have resulted in a paradigm shift in medical education [34]. Teaching a technical skill is processed by the following 4 steps: 1) demonstration: show how to perform a procedure instead of using explanations; 2) analysis: explains each step; 3) understanding: trainee performs a procedure while trainer explains; and 4) performance: trainee performs and explains the procedure.
Although animals and cadavers can be used to teach technical skills for medical students, utilization of simulators for technical skill training has become a major trend in recent years [35]. Simulation has been recognized as a useful method in acquiring technical skills because simulation fits well with the three-stage model of cognition, integration and automation [35]. Cognition is developing an understanding of the task, and being able to make a clear description and demonstration of the task. Integration makes knowledge obtained from the cognition to be incorporated into learning the motor skills for the task. Finally, the task becomes automatic and even subconscious. Competence in procedural skills is achieved by a variable number of attempts in normal and pathological conditions, and depends on the quality of teaching, motor skills and aptitude of individual trainees. Pre-trained novice can obtain proficiency without direct patient contact. If a learner reaches the level of automation in performing certain procedure, he or she can achieve additional abilities such as communication, teamwork and decision making [36].
Procedural skill assessment is generally considered less important than knowledge and judgment [37]. Parts of anatomical area trainers have been used for procedural skill training instead of high fidelity full-scale computer based simulators. Part of anatomical area trainers are widely used because it is less expensive than full scale patient simulators. However, full scale simulators can simulate better in the settings of anesthesia clinical skill teaching which needs indispensable, quick and accurate performance at critical situation [38].
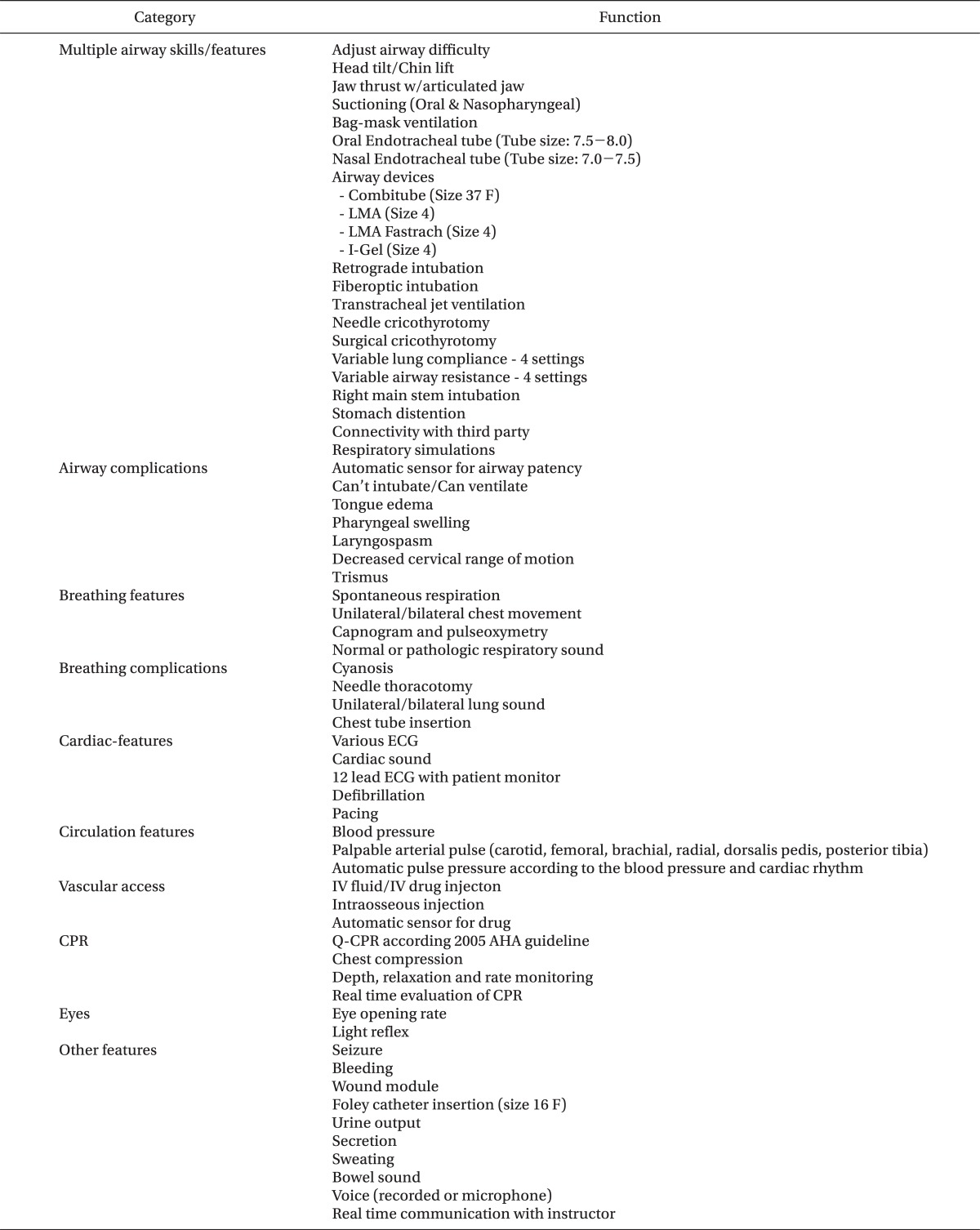
A type of full scale simulator function is described in Table 1. Hybrid simulation, a combination of a standardized patient who plays a role of assessing communication skills and a manikin simulator which assesses technical skills, is also useful in anesthesia procedural skill training. Therefore, the development of more realistic simulation programs will provide more complex and higher quality education on both technical and non-technical skills.
High fidelity simulators provide more realistic simulation environment and educational effects in comparison to simple part trainers. Therefore, it is essential to facilitate high fidelity simulators and to replicate various simulation programs.
Non-technical skills can be defined as cognitive, social, and personal resource skills that complement technical skills, and contribute to safe and efficient task performance [39]. Adverse event data from anesthesia showed that non-technical skills play a key role in patient safety. A review of human factors and current use of behavioral markers, questionnaire survey, problems and concerns, observations in theatre, and interviews with consultant anesthetists to identify the non-technical skill underpinning their practice were undergone.
For example, anesthesiologists and psychologists designed the anesthesia non-technical skills (ANTS) system using task analysis similar to the non-technical skills (NOTECHS) system for pilots. NOTECHS is applied first in pilot training. Non-technical skills are also applied in surgery, and assessment of surgical non-technical skills (NOTSS) is becoming a training priority to develop in surgeons. The present evidence suggests that the revised NOTSS exhibits good reliability [40]. NOTSS is consisted of 4 categories, situation awareness, decision making, communication and teamwork, and leadership. Such tools like NOTECHS and NOTSS may be helpful in the development of non-technical skill training in anesthesiology. Such non-technical skills should be developed according to the regional and cultural environment.
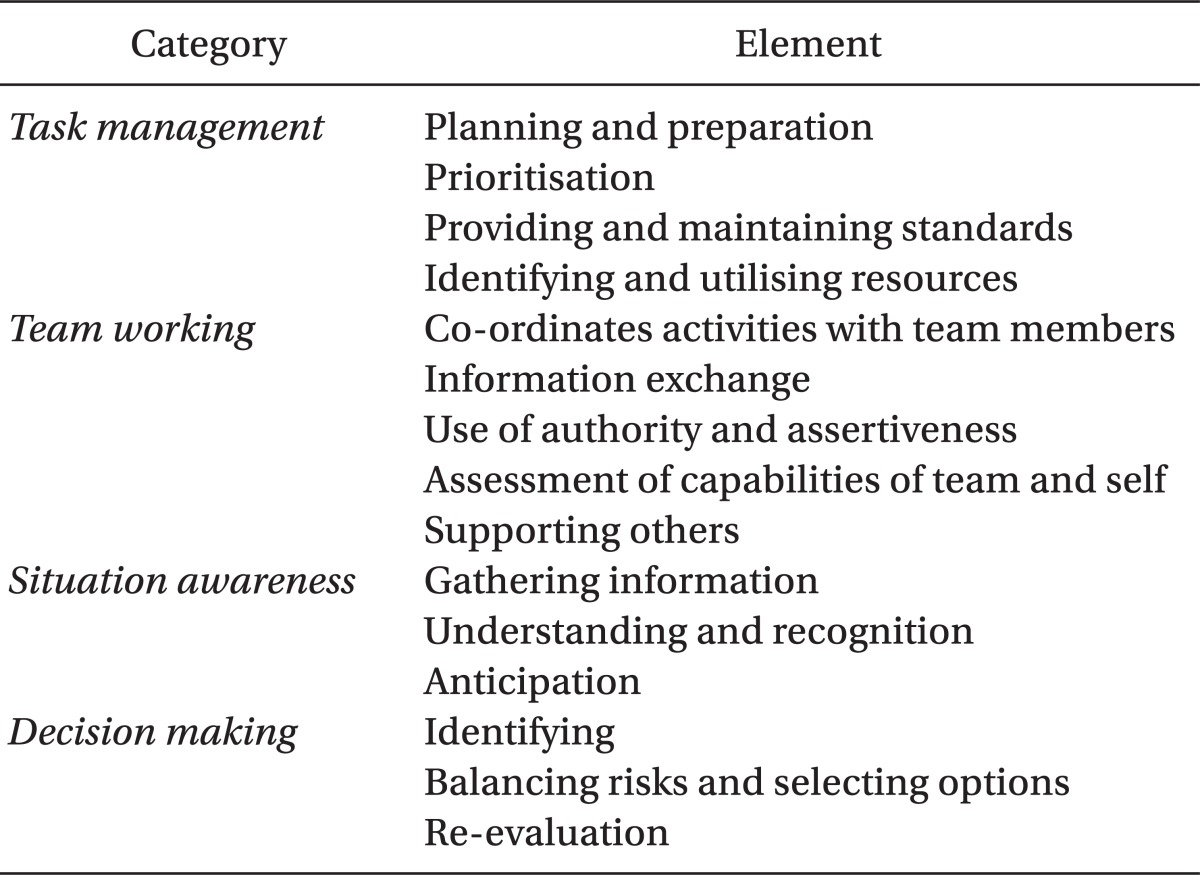
ANTS is a type of non-technical skill training tool consisting of 4 categories with each category having 3 to 5 elements [41]. The four categories are task management, team working, situation awareness, and decision making (Fig. 2). Each element is assessed by a behavior marker. Task management is the skill of management of resources and organization of tasks to achieve goals, be they individual case plans or longer term scheduling issues. It contains 4 elements, namely planning and preparation, prioritization, providing and maintaining standards, and identifying and utilizing resources. Team working is the skill of working with others as a team, in any role, to ensure effective joint task completion and team satisfaction; the focus is on the team rather than the task. It has 5 elements, namely coordinate activities with team members, information exchange, the use of authority and assertiveness, assessment of capabilities of team and self, and supporting others. Situation awareness is the skill of developing and maintaining an overall dynamic awareness of the situation based on the perception of elements of the theatre environment; that is, understanding what they mean and thinking ahead about what could happen in the near future regarding the patient, team, time, displays, and equipment. It has 3 elements, namely gathering information, understanding and recognition, and anticipation. Decision making is the skill of making decisions to reach a judgment or diagnosis about a situation, or to select a course of action, based on experience or new information under both normal conditions and in time-pressured crisis situations. It has 3 elements, namely identifying, balancing risks and selecting options, and re-evaluation (Table 2) [42].
Behavioral markers are rated as either positive or negative result. For example, in the planning and preparation element of task management, good practices are communicate plan for case relevant staff, review case plan in light of changes and make post-operative arrangements for the patient. Poor practices of planning and preparation are do not adapt plan in light of information, do not ask for drugs or equipment until the last minute, do not have emergency or alternative drugs available for the patient, and fail to prepare theater.
ANTS is applied to simulators and in-theatre training to assess non-technical skills, to identify trainee's competence, to give structured feedback, and to inform further training. The ANTS framework can be used for post- scenario or operation debriefing [43]. The purposes of evaluation of non-technical skills are feedback, testing skills or licensing, the efficacy of nontechnical skills training programs and constructing databases and analyses.
Simulation has a potential to promote a new paradigm compared to traditional education tools. Technical skills and non-technical skills can be taught to anesthesiology residents via a standardized and organized simulation program. Such programs would be beneficial in training anesthesia teams working in the operation room.
In conclusion, academic societies should develop simulation programs that are compatible with the international standards and periodic demand to achieve clinical competency and patient safety thorough medical education based on simulation.
References
1. Gaba DM, Howard SK. Simulated anaesthetic emergencies. Br J Anaesth 1997; 79: 689-690. PMID: 9422915.


2. Denson JS, Abrahamson S. A computer-controlled patient simulator. JAMA 1969; 208: 504-508. PMID: 5818529.


3. Gordon MS. Cardiology patient simulator. Development of an animated manikin to teach cardiovascular disease. Am J Cardiol 1974; 34: 350-355. PMID: 4136577.


4. Karnath B, Thornton W, Frye AW. Teaching and testing physical examination skills without the use of patients. Acad Med 2002; 77: 753PMID: 12114177.

5. Philip JH. Gas Man--an example of goal oriented computer-assisted teaching which results in learning. Int J Clin Monit Comput 1986; 3: 165-173. PMID: 3540162.


6. Merril GL, Barker VL. Virtual reality debuts in the teaching laboratory in nursing. J Intraven Nurs 1996; 19: 182-187. PMID: 8852175.

7. Chopra V, Gesink BJ, de Jong J, Bovill JG, Spierdijk J, Brand R. Does training on an anaesthesia simulator lead to improvement in performance? Br J Anaesth 1994; 73: 293-297. PMID: 7946851.



8. Gaba DM, Howard SK, Flanagan B, Smith BE, Fish KJ, Botney R. Assessment of clinical performance during simulated crises using both technical and behavioral ratings. Anesthesiology 1998; 89: 8-18. PMID: 9667288.


9. Rogers PL, Jacob H, Thomas EA, Harwell M, Willenkin RL, Pinsky MR. Medical students can learn the basic application, analytic, evaluative, and psychomotor skills of critical care medicine. Crit Care Med 2000; 28: 550-554. PMID: 10708198.


10. Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach 2005; 27: 10-28. PMID: 16147767.


11. Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA 2011; 306: 978-988. PMID: 21900138.


12. Cooper JB, Taqueti VR. A brief history of the development of mannequin simulators for clinical education and training. Postgrad Med J 2008; 84: 563-570. PMID: 19103813.


13. Park CS, Rochlen LR, Yaghmour E, Higgins N, Bauchat JR, Wojciechowski KG, et al. Acquisition of critical intraoperative event management skills in novice anesthesiology residents by using high-fidelity simulation-based training. Anesthesiology 2010; 112: 202-211. PMID: 20010420.


14. Castanelli DJ. The rise of simulation in technical skills teaching and the implications for training novices in anaesthesia. Anaesth Intensive Care 2009; 37: 903-910. PMID: 20014595.


15. Kneebone R. Simulation in surgical training: educational issues and practical implications. Med Educ 2003; 37: 267-277. PMID: 12603766.


16. Kneebone R. Evaluating clinical simulations for learning procedural skills: a theory-based approach. Acad Med 2005; 80: 549-553. PMID: 15917357.


17. Smith CC, Huang GC, Newman LR, Clardy PF, Feller-Kopman D, Cho M, et al. Simulation training and its effect on long-term resident performance in central venous catheterization. Simul Healthc 2010; 5: 146-151. PMID: 20651476.


18. Park CS, Rochlen LR, Yaghmour E, Higgins N, Bauchat JR, Wojciechowski KG, et al. Acquisition of critical intraoperative event management skills in novice anesthesiology residents by using high-fidelity simulation-based training. Anesthesiology 2010; 112: 202-211. PMID: 20010420.


19. Kremer MJ, Faut-Callahan M, Hicks FD. A study of clinical decision making by certified registered nurse anesthetists. AANA J 2002; 70: 391-397. PMID: 12425129.

20. Cooper GM, McClure JH. Anaesthesia chapter from Saving mother's lives; reviewing maternal deaths to make pregnancy safer. Br J Anaesth 2008; 100: 17-22. PMID: 18070784.



21. Draycott T, Sibanda T, Owen L, Akande V, Winter C, Reading S, et al. Does training in obstetric emergencies improve neonatal outcome? BJOG 2006; 113: 177-182. PMID: 16411995.


22. Okuda Y, Bond W, Bonfante G, McLaughlin S, Spillane L, Wang E, et al. National growth in simulation training within emergency medicine residency programs, 2003-2008. Acad Emerg Med 2008; 15: 1113-1116. PMID: 18717652.


23. Borges BC, Boet S, Siu LW, Bruppacher HR, Naik VN, Riem N, et al. Incomplete adherence to the ASA difficult airway algorithm is unchanged after a high-fidelity simulation session. Can J Anaesth 2010; 57: 644-649. PMID: 20440663.


24. Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JH, McGaghie WC. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest 2008; 133: 56-61. PMID: 17573509.


25. Barsuk JH, McGaghie WC, Cohen ER, O'Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med 2009; 37: 2697-2701. PMID: 19885989.


26. Bruppacher HR, Alam SK, LeBlanc VR, Latter D, Naik VN, Savoldelli GL, et al. Simulation-based training improves physicians' performance in patient care in high-stakes clinical setting of cardiac surgery. Anesthesiology 2010; 112: 985-992. PMID: 20234305.


27. Duncan JR, Henderson K, Street M, Richmond A, Klingensmith M, Beta E, et al. Creating and evaluating a data-driven curriculum for central venous catheter placement. J Grad Med Educ 2010; 2: 389-397. PMID: 21976088.



28. Merli G, Guarino A, Della Rocca G, Frova G, Petrini F, Sorbello M, et al. Recommendations for airway control and difficult airway management in thoracic anesthesia and lung separation procedures. Minerva Anestesiol 2009; 75: 59-96. PMID: 18987567.

29. Kuduvalli PM, Jervis A, Tighe SQ, Robin NM. Unanticipated difficult airway management in anaesthetised patients: a prospective study of the effect of mannequin training on management strategies and skill retention. Anaesthesia 2008; 63: 364-369. PMID: 18336486.


30. Houben KW, van den Hombergh CL, Stalmeijer RE, Scherpbier AJ, Marcus MA. New training strategies for anaesthesia residents. Curr Opin Anaesthesiol 2011; 24: 682-686. PMID: 21971397.


31. Murray DJ. Current trends in simulation training in anesthesia: a review. Minerva Anestesiol 2011; 77: 528-533. PMID: 21540808.

32. Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthc 2007; 2: 115-125. PMID: 19088616.


33. Arora S, Ahmed M, Paige J, Nestel D, Runnacles J, Hull L, et al. Objective structured assessment of debriefing: bringing science to the art of debriefing in surgery. Ann Surg 2012; 256: 982-988. PMID: 22895396.


34. Bould MD, Crabtree NA, Naik VN. Assessment of procedural skills in anaesthesia. Br J Anaesth 2009; 103: 472-483. PMID: 19720612.



35. Reznick RK, MacRae H. Teaching surgical skills--changes in the wind. N Engl J Med 2006; 355: 2664-2669. PMID: 17182991.


36. Satava RM. Mental workload: a new parameter for objective assessment? Surg Innov 2005; 12: 79PMID: 15846450.


37. Tetzlaff JE. Assessment of competency in anesthesiology. Anesthesiology 2007; 106: 812-825. PMID: 17413920.


38. Vadodaria BS, Gandhi SD, McIndoe AK. Comparison of four different emergency airway access equipment sets on a human patient simulator. Anaesthesia 2004; 59: 73-79. PMID: 14687103.


39. Flin R, Maran N. Identifying and training non-technical skills for teams in acute medicine. Qual Saf Health Care 2004; 13(Suppl 1): i80-i84. PMID: 15465960.



40. Yule S, Flin R, Maran N, Rowley D, Youngson G, Paterson-Brown S. Surgeons' non-technical skills in the operating room: reliability testing of the NOTSS behavior rating system. World J Surg 2008; 32: 548-556. PMID: 18259809.


41. Patey R, Flin R, Fletcher G, Maran N, Glavin R. Edited by Henriksen K, Battles JB, Marks ES, Lewin DIDeveloping a Taxonomy of Anesthetists' Nontechnical Skills (ANTS). Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products). 2005, : Rockville (MD), Agency for Healthcare Research and Quality (US).

42. Flin R, Patey R, Glavin R, Maran N. Anaesthetists' non-technical skills. Br J Anaesth 2010; 105: 38-44. PMID: 20522911.



43. Fletcher G, Flin R, McGeorge P, Glavin R, Maran N, Patey R. Anaesthetists' Non-Technical Skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth 2003; 90: 580-588. PMID: 12697584.



- TOOLS