Ultrasound visibility of regional anesthesia catheters: an in vitro study
Article information
Abstract
Background
Ultrasound subjective visibility of in-plane needles is correlated with the intensity difference between the needle surface and the background. Regional anesthesia catheters are difficult to visualize by an ultrasound. In the present study, we investigated the ultrasound visibility of the catheters.
Methods
Six catheters were placed at 0° and 30° relative to and at a depth of 1 cm below the pork phantom surface. Ultrasound images of in-plane catheters were evaluated, subjectively and objectively. Outer and inner objective visibilities were defined as the difference in the mean pixel intensity between the catheter surface and adjacent background, and between the surface and the center of the catheter, respectively. Evaluations were made based on the portion of the catheters. A P value < 0.05 was considered significant.
Results
Subjective visibility was more strongly correlated with the inner objective visibility than with the outer objective visibility at both angles. Metallic 19-gauge catheters were more subjectively visible than the non-metallic 20-gauge catheters at 30° degrees (P < 0.01). Subjective, and outer and inner objective visibility were significantly lower at 30° than at 0° (P < 0.01, P < 0.01, P = 0.02). Perifix ONE at 0° and Perifix FX at 30° were the most visible catheters (P < 0.01 for both).
Conclusions
Subjective visibility of catheters can not be evaluated in the same manner as that of the needles. For the best possible visualization, we recommend selecting a catheter with a structure that enhances the dark at the center of catheter, rather than basing the catheter selection on the bore size.
Introduction
There have been several studies on the ultrasound visibility of non-textured needles for the use in regional anesthesia [1,2]. Ultrasound-guided nerve blocks performed with non-textured needles have better success rates than that of the traditional methods of nerve blocking, such as fluoroscope-guided, and landmark approach [3-7]. The subjective visibility of in-plane needles is reported to be correlated with the intensity difference between the needle surface and the background [8].
Although conventional regional anesthesia catheters need to be positioned precisely beside the target nerve, they are difficult to visualize by ultrasound [9-11]. The relative ultrasound visibility of commonly used catheters has not been previously reported. In the present study, we assessed the ultrasound visibility of a variety of catheters, and determined the impact of catheter width and angle on the visibility in vitro.
Materials and Methods
Catheters
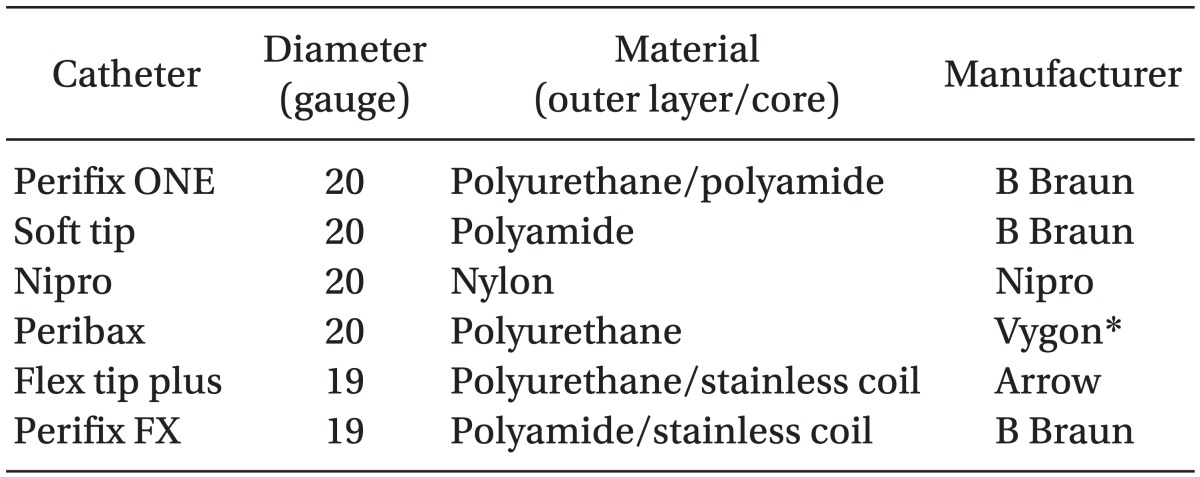
We examined 6 catheters that are commonly used for ultrasound-guided regional anesthesia in Japan (Table 1).
Ultrasound equipment
We used a nerve block-specific ultrasound device S-Nerve, with linear probe: HFL38x 13-6 MHz, (SonoSite Inc., Bothell, WA, USA) in this study, with the examination type set to "Nerve" mode. The gain was not adjusted after start-up, and neither were any other configurations.
Phantom
Because anatomic structures of a pork phantom are clearly visualized with an ultrasound, including the background echogenicity, tissue layers, and needle images that are comparable to those in the human tissue [12], we used a boneless pork phantom (10 × 10 × 20 cm).
Study protocol
Catheters were primed with saline. We placed catheters at 0° and 30° relative to the pork phantom surface at a depth of 1 cm below the upper surface of the pork phantom to the probe surface. All catheters were inserted in-plane with a needle guide (Infiniti, CIVCO Medical Solutions, Kalona, IA, USA), using the needles provided in the respective catheterization kits. We avoided prior traces when inserting the catheters. Each catheter was placed as straight as possible to minimize the influence of winding on the visibility. All images of the catheters were digitally recorded to the hard disk to analyze at a later time. We inserted 10 catheters of each type into the pork phantoms, using this procedure.
Image evaluation
Assessment of the acquired images was performed using Photoshop Elements (Version 7.0; Adobe Systems, San Jose, CA, USA) by an investigator who was not involved to the blinding of the catheter type. Images were placed in random order, and the ultrasound visibility was evaluated according to the methods described by Schafhalter-Zoppoth et al. [8], with modifications. Pixel intensity was defined as the gray-scale value between 0 (black) and 255 (white). The outer objective visibility (pixel intensity units [PIUs]) was estimated by the difference in the mean pixel intensity between the surface of the catheter and the adjacent background. We also measured the outer objective visibility of the brightest tissue on each image. We defined the inner objective visibility as the difference in the mean pixel intensity between the surface and the center of the catheter. Negative values indicate that the center was brighter than that of the surface, and the catheter looked like a graded white line. Positive inner objective visibility values indicate that the center of the catheter was darker than the edges, and the catheter appeared as white parallel lines. Subjective visibility (subjective visibility units, [SVUs]) is a measure of the recognizability of the lines on the image as a catheter. SVUs fall on a scale ranging from 0 to 3 (0 = invisible, 1 = poor, 2 = good, 3 = excellent), and were scored in 0.5 increments by 10 anesthesiologists. Evaluations were made based on the portion of the catheter, which was 1 cm deep at 30o relative to the surface of the pork phantom.
Statistical analysis
Unpaired t tests were used to compare the continuous variables, Wilcoxon signed-rank tests were used to compare the ordinal variables, and single-factor ANOVA was used in multivariate analyses. All statistics were calculated using StatView (Version 4.54, SAS Institute Inc., Cary, NC). A P value < 0.05 was considered statistically significant. Data are presented as the mean ± SD.
Results
Catheter
Fig. 1 shows a sample image of each catheter. At 0°, the mean outer objective visibility of all catheters was significantly higher than that of the brightest tissue (119 ± 27 PIU vs. 81 ± 19 PIU, P < 0.01). Visibility measures for the tested catheters are shown in Fig. 2. Among the catheters tested, Perifix ONE had the highest subjective and inner objective visibility scores. The outer objective visibility was not significantly different between the catheters. At 30°, the outer objective visibility of all catheters was comparable to that of the brightest tissue (79 ± 16 PIU vs. 80 ± 17 PIU, P = 0.66). Among the catheters tested, Perifix FX had the highest subjective and inner objective visibility. The outer objective visibility was not significantly different between the catheters (Fig. 2).

Visibility of the catheters at 0° (A-C) and 30° (D-F). (A, D) Subjective visibility. (B, E) Outer objective visibility. (C, F) Inner objective visibility. Data are shown in mean ± SD. P < 0.05 is considered significant. *vs. Perifix ONE at 0°, †P vs. Perifix FX at 30°, ‡vs. Flex tip plus at 30°.
Subjective visibility was more strongly correlated with the inner objective visibility than with the outer objective visibility, at both 0° (R2 = 0.79, P < 0.01 vs. R2 = 0.11, P = 0.49) and 30° (R2 = 0.66, P < 0.01 vs. R2 = 0.21, P = 0.27) (Fig. 3).
Catheter diameter
At 0°, there was no significant difference in any visibility measures between the catheters of different diameter. At 30°, subjective and inner objective visibilities of 19-gauge catheters were significantly greater than those of the 20-gauge catheters (Table 2).
Angle
All visibility measures were significantly lower at 30° than at 0° (subjective visibility 1.7 ± 0.5 SVU vs. 1.2 ± 0.3 SVU, P < 0.01; outer objective visibility 119 ± 27 PIU vs. 78 ± 16 PIU, P < 0.01; inner objective visibility 3.5 ± 22 PIU vs. -4.9 ± 18 PIU, P = 0.02).
Discussion
Catheter
Observers were able to recognize every catheter as a catheter at both angles of the insertion. The surface brightness does not contribute to the subjective visibility, although, the needle brightness does. The positive inner objective visibility values of Perifix ONE and Perifix FX, indicate a relatively dark center, which probably helps to make it more visible at both angles. According to the manufacturer, neither of these catheters is designed for ultrasound visibility. Some particular combinations of the materials and their thickness change the reflectivity of an ultrasound beam and may enhance the dark at the center of the catheter, as reported in the study of the needle visibility, enhanced by the insertion of a guide wire [8].
Catheter diameter
Although both 19-gauge catheters are metallic, they were not any more visible at 0° than the 20-gauge non-metallic catheters. At 30°, the 19-gauge catheters were better visualized than the 20-gauge catheters. This difference is not due to the width of the catheter because the width did not contribute to the subjective visibility at 0°. The difference in the visibility between these two catheter sizes is more likely to be due to the differences in the materials used to manufacture them, as the 19-gauge catheters produced the inner objective visibility that was greater than 0.
Angle
The brightest needle images are obtained when the ultrasound beam reflects perpendicular to the needles [1,8]. This is also true for the catheters, as the outer objective visibility declines as the insertion angle increases. The resulting decrease in the inner and outer objective visibility may cause an observed decline in the subjective visibility.
A non-textured needle appears as a bright straight line, with acoustic shadows on an ultrasound image [13], which is unlike any biostructure. Therefore, it is distinguishable from the surrounding tissue. However, at a steep insertion angle, visualization of non-textured needles is challenging [14-16]. Recent studies have indicated that the echogenic needles have better visibility and a higher rate of success than the non-textured needles [17,18]. In contrast, catheters generally appear as dark curves or short segments without acoustic shadows, and sometimes, resemble fascia, fat, or other tissues. Subjective catheter visibility is influenced by the inner objective visibility at both 0° and 30°, and methods for enhancing the ultrasound visibility of catheters are needed.
In the present study, we did not focus on the visibility of the catheter tip, which directly affects the success of nerve blockades. However, the winding of the catheter tips make it challenging to make a distinction between them from a surface cross-section in still images. Therefore, we recommend a dynamic assessment [19,20] in future studies. This study was limited by the placement of catheters only at the shallow sites. Placement at deeper sites results in lower surface intensities and may lead to poor inner objective visibility. We examined the visibility only at limited angles, while we found that it was difficult to delineate catheters placed at angles > 45°, relative to the probe surface in a preliminary study (data not shown). Although the axial or cross-section images of catheters are more easily available in clinical settings, we examined the in-plane images in this study for the best possible visibility of the catheters. Our study was also limited by the inclusion of only the catheters made of different materials. No catheters with texturing or with electric stimulation are available, at present. Although the comparison between the 2 size catheters, made of the same material, would draw a more lucid conclusion, we could obtain only 6 different material catheters for this study. Comparisons among other catheter types are necessary in order to determine the best catheters for use in ultrasound-guided nerve blocks.
In conclusion, some of the catheters are recognizable when placed at either 0° or 30°. Unlike the subjective needle visibility, the subjective catheter visibility is influenced more by the inner objective visibility than that of the outer objective visibility. For the best possible visualization, we recommend selecting a catheter with a structure that enhances the dark at the center of catheter, rather than basing catheter selection on the bore size. Placing catheters at shallow angles and as straight as possible improves visualization. This is the first report of the ultrasound visibility of catheters that are used in regional anesthesia.