A comparison between caudal block versus splash block for postoperative analgesia following inguinal herniorrhaphy in children
Article information
Abstract
Background
We wanted to determine the postoperative analgesic efficacy of preincisional caudal epidural block versus instillation (splash block) following inguinal herniorrhaphy in children.
Methods
Thirty children (age range: 1-7 years) who were scheduled to undergo inguinal herniorrhaphy were divided into 2 groups: the caudal block group and the splash block group with 15 children in each group. Tracheal intubation was performed. Fifteen children received caudal block with 1.0 ml/kg of 0.25% ropivacaine (Group 1). Caudal block was performed using the loss of resistance method via the sacral hiatus. Fifteen children in Group 2 received local instillation (splash block) in the surgical site with up to 0.4 ml/kg of 0.25% ropivacaine. The patients were observed for 90 minutes in the postanesthesia care unit and then they were transferred to the ward. The pain scores were taken 4 times. We assessed pain using the Faces pain scores.
Results
There were no significant differences between the groups regarding the pain scores at 10, 30 and 60 minutes upon entering the postanesthesia care unit. The pain scores of Group 1 were slightly lower at the last evaluation point when compared to that of Group 2. One patient in Group 1 required supplemental postoperative intravenous (IV) tramadol, while all the other patients in both groups did not require supplemental IV tramadol. The intraoperative requirement for sevoflurane was decreased in Group 1 as compared to that of Group 2. There were no major complications related to either type of block.
Conclusions
We conclude that a splash block can have a similar analgesic effect as that of a caudal block for the postoperative herniorrhaphy pain of children.
Introduction
Pediatric caudal block was first introduced in 1933 by Cambell, and since then it has become more frequently used because it can be used in anesthesia for inguinal and perineal surgery, it has postoperative analgesic effects, it allows for early ambulation and it has the advantage of reducing the required doses of inhalational anesthetics when used in combination with general anesthesia [1]. However, the blood vessels in the sacral space are well-developed, so there are cases when needle aspiration does not draw out blood even when the tip of the needle is inside the blood vessel, so there is always the possibility of systemic toxicity due to local anesthetics. Because of the limitations of this procedure, a different method of pain control is needed for the cases with a central nervous disorder, spinal deformity, inflammation of the block site or a coagulation disorder.
Many studies have been conducted to find substitutes for caudal blocks such as the ilioinguinal-iliohypogastric nerve block and infiltrations of local anesthetics. These methods are similar to caudal block as they are characterized by postoperative analgesia, but they are not widely used because they are difficult procedures and they can create postprocedural anatomical structural distortions [2-4].
On the other hand, splash blocks, which is an altered form of the ilioinguinal-iliohypogastric nerve block, is a simple analgesic method with no side-effects. The hernial sacs are ligated when performing herniorrhaphies and local anesthetics are instilled into the incision site before closing it so that the local anesthetics are absorbed into the muscular coat and the exposed nerves [4].
The purpose of this study is to compare the analgesic effect of caudal blocks and splash block when performing pediatric inguinal herniorrhaphies.
Materials and Methods
Thirty ASA I and II patients (1-7 years of age and less than 25 kg in weight) who were scheduled for an inguinal herniorrhaphy under general anesthesia at our hospital were included in the present study. Fifteen patients were placed in each group. Group 1 received a caudal block, and Group 2 received a splash block. The patients with pulmonary disorders, respiratory disorders, nervous disorders, spinal deformities, skin disorders or coagulation disorders at the injection site were excluded from the study. This study was approved by the ethics committee of our hospital. After our explanation to the guardians of the patients about the study, they gave us their written consent. We informed them about the postoperative requirement for cooperation.
Glycopyrrolate 0.004 mg/kg as premedication was administered IM to all the patients 30 min prior to surgery. Measurements of the EKG, pulse-oxymetry and noninvasive blood pressure monitoring were performed when the patient was on the operating table, and the vital signs were monitored too. For anesthetic induction and endotracheal intubation, propofol 2 mg/kg and rocuronium 0.6 mg/kg mixed with lidocaine 0.1 mg/kg were IV administered while monitoring the vital signs. Oxygen at 1 L/min, air at 2 L/min, and sevoflurane 1.5-2.0 vol% were used for maintaining the anesthesia. After the caudal block was performed in Group 1, anesthesia was maintained with sevoflurane 1.0-1.5 vol%.
For the caudal block, the patients were first intubated and then they were placed in the altered left lateral position. The block site, which was mainly at the sacral hiatus, was sterilized with betadine, and the sacral hiatus between the sacral conui was palpated. Then a 23-gage short needle injection was used with the bevel towards the abdomen to puncture the sacral surface at a 45-degree angle. When the sacrococcygeal ligament seemed to have punctured, the needle was tilted more towards the skin surface and the needle was inserted 2-3 mm deeper. The needle was aspired to check for blood and cerebral spinal fluid extravasations. The loss of resistance was confirmed with air-infusion. Then 0.25% ropivacaine 1 ml/kg was infused.
For the splash block, 0.25% ropivacaine 0.4 ml/kg was prepared and the hernial sac was ligated. Before closing the incision site, 0.2 ml/kg of 0.25% ropivacaine was instilled. The muscular coat was sutured and at the end 0.1 ml/kg 0.25% ropivacaine was instilled before suturing the subcutaneous tissue. Adequate instillation was performed similar to how the wound site was sterilized. The instilled state was maintained for a minimum of 1 minute each time. Gauze cleaning was skipped so that the local anesthetics could adequately be absorbed.
After the surgery and when the return of spontaneous respiration was confirmed, glycopyrrolate 0.008 mg/kg and pyridostigmine 0.2 mg/kg were IV administered and then the patient was extubated. The same anesthesiologist performed all the caudal blocks. All the splash blocks were performed by a surgeon who was knowledgeable of the surgery's objectives and methods in advance.
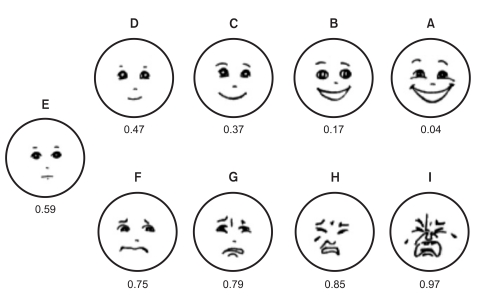
For postoperative pain evaluation, the pain scores were measured and the facial pain scores (Fig. 1) were taken 10 min, 30 min and 60 min upon arriving into the PACU. The patients were moved to their wards after 90 min passed in the PACU. At 120 min post-surgery, the last pain scores were taken. The pain scores were taken when the patient was not crying. If the pain score was over 0.6, then tramadol 1.2 mg/kg was infused.
Data analysis was done by using SPSS ver. 7.0 for Windows. Because the sample score was low, it was difficult to assume a normal distribution for the population. So, the Mann-Whitney test was used to evaluate the differences between the two groups. P values below 0.05 were considered significant.
Results
The study set the general conditions of the 30 test-patients as ASA I or II with 15 patients to receive a caudal block and 15 to receive a splash block. There were no significant differences between the patients for age, weight or gender. The anesthesia time in Group 1, including the surgery time, was a minimum of 55 minutes to a maximum of 90 minutes. For Group 2 it was a minimum of 55 min to maximum of 105 minutes. The extubation time in Group 1 was on average 12.6 minutes; for Group 2 it was on average 12.8 minutes. There were no significant differences between the two groups (Table 1).
There were no side-effects such as postoperative vomiting and respiratory disorder observed in Group 1 or Group 2 after the procedure in this study.
Ten min, 30 min and 60 min upon arriving into the PACU, the pain scores were taken, as are shown in Table 2. Group 1 had lower scores compared with that of Group 2, but the P values 0.343, 0.104, and 0.168 showed no statistically significant differences. Thirty min upon arriving into the ward, the pain score in Group 1 was 0.51 ± 0.34, which was lower than Group 2's (0.55 ± 0.49). The P value was 0.019, and this was statistically significant. During the pain evaluation period, a supplemental dose of tramadol was used once in Group 2, but none were used in Group 1. The patients were discharged 2-3 days after being in the ward without using additional analgesics.
Discussion
Taddio et al. reported that newborn babies who experience pain will have altered behavior in their childhood, and so the purpose of pain control is not pain alleviation, rather, it is to prevent pain [5]. For children who undergo a herniorrhaphy, the methods of postoperative general pain control include the IV administration of nonopioid anesthetics or opioid anesthetics, and many other nerve block procedures. Opioid anesthetics are related to vomiting or prolonged anesthesia awareness, and their use eventually leads to delayed discharge from the hospital [6]. For caudal blocks children have less local subcutaneous fat than adults, so the sacral hiatus is easily palpated and this makes the procedure simpler. Because caudal blocks have almost a zero failure rate, its perioperative and postoperative effects on the cardiovascular system are minor. Caudal blocks can effectively control pain since the required dose of perioperative general anesthetics can be reduced and the postoperative recovery is rapid [7-9]. However, complications of regional anesthesia do exist such as bone marrow puncture, intestinal damage and the danger of an increase of the blood concentration, and these complications can lead to system toxicity. Central nervous disorders, spinal deformities, inflammation of the block site and coagulation disorders are counter-indications for regional anesthesia, so it is necessary to find a substitute to control pain [10].
Hannallah et al. proved that there are no differences in the postoperative analgesic effects between caudal blocks and ilioinguinal-iliohypogastric nerve blocks post-orchiorrhaphy. After ligating the inguinal hernia, they found that local anesthetic infiltration at the incision site showed the same postoperative analgesic effect as caudal blocks [2-4]. Roy-Shapira et al. stated that ilioinguinal-iliohypogastric nerve blocks are linked with the risks of temporarily paralysis of the quadriceps, hematoma and spontaneous intestinal perforation [11]. Casey et al. stated that in 30 pediatric patients who underwent herniorrhaphy, after the hernia sac was ligated, the incision site was instilled with 0.25% bupivacaine 0.25 ml/kg, and this was just as effective for pain control as an ilioinguinal-iliohypogastric nerve block [3]. However after the ligature, the local infiltration distorted the child's anatomical structure [12], Therefore, surgeons are hesitant to perform local infiltration. On the other hand, splash blocks are simple and they can be easily used in cases where caudal blocks cannot be performed, and they have virtually no side-effects. Further, there is no possibility of distortions of the anatomical structure due to local infiltration, and this advantage that will spur surgeons to use slash blocks.
In the present study, no complications such as postoperative vomiting or respiratory disorder were observed after the procedure in either Group 1 or Group 2 [13-15]. There were no significant statistical differences found in the pain scores measured at 10 min, 30 min and 60 min after arriving into the PACU. In Group 2, an additional dose of tramadol was used, but a postoperative analgesic effect similar to caudal anesthesia was visible all the other patients in both groups. The pain scores measured 120 min post-surgery were statistically lower in Group 1 as compared to that of Group 2. No additional anesthetics were used in either of the 2 groups up to the point of discharge from the hospital. Such results can be interpreted that the caudal block, as compared to the splash block, is more effective in managing postoperative pain and that the effects of pain alleviation from a caudal block last longer. However, we did not evaluate the pain scores from postoperative 120 min to the point of discharge. Also, the ward conditions were not consistent among the patients. Moreover, no accurate studies have been done on the psychological effects or the analgesic duration of caudal blocks and splash blocks, and so this requires further research.
Casey et al. [3] compared the analgesic effects of splash block using 0.25% bupivacaine 0.25 ml/kg and ilioinguinal-iliohypogastric nerve blocks in 2-10 year-old patients who underwent inguinal herniorrhaphy. They found that there were was no differences of the pain scores, recovery time and time till discharge. For the splash block, the hernial sac was ligated and the incision site was adequately instilled and maintained for 2 min in that state before closing. The muscular coat was closed, and then the instillation was performed and maintained in that state for 2 min with the same methods. Conroy et al. [16] compared the analgesic effect of splash blocks with 0.25% bupivacaine 0.5 ml/kg mixed with epinephrine 5 µg/ml with that of caudal blocks using bupivacaine 0.75 ml/kg of the same concentration in 2-month to 10-year-old children who were undergoing inguinal herniorrhaphy. They found that caudal blocks, as compared to splash blocks were superior for the extubation time, the analgesic effects and the discharge time. The splash block was performed in the same manner as used by Casey et al.
Machotta et al. [17] compared the analgesic effects of splash blocks for 24 hrs using 0.5% bupivacaine 0.2 ml/kg to that of caudal blocks using 0.25% bupivacaine 1 ml/kg in 0-5 year-old children who were undergoing inguinal herniorrhaphy. They found that the two groups had no statistical differences for the dose of analgesics, the discharge time and the postoperative pain scores. In the present study, the caudal blocks were performed after the end of the surgery and extubation, whereas the splash blocks were performed after the fascia transversalis was closed.
In the present study, the caudal block was performed after anesthetic induction with 0.25% ropivacaine 1 ml/kg and before surgery. For the splash block, 0.25% ropivacaine 0.4 ml/kg was used when ligating the hernial sac. Before closing the incision site, 0.2 ml/kg of 0.25% ropivacaine was instilled. The muscular coat was sutured and 0.1 ml/kg of 0.25% ropivacaine was instilled for the last time into the subcutaneous tissue before suturing. Thus, instillation was performed a total of 3 times. Instillation was adequately performed in the same manner as wound sterilization, and the instilled state was maintained for at least 1 min each time. In the study performed by Machotta et al., the caudal block was performed after the surgery and after extubation, whereas the splash block was performed in a similar manner as that of the caudal block, but with twice the concentration of the local anesthetics. The present study used 0.25% ropivacaine as the local anesthetic. The caudal block was performed after anesthetic induction and before surgery. The pain scores were observed at only 120 minutes post-surgery. Only additional anesthetics were used until the point of discharge. The pain scores were constant until 60 min post-surgery, but the pain scores at 120 min post surgery were significantly decreased in Group 1. It is estimated that perioperative pain stimulation due to the types and concentrations of the local anesthetics used for splash blocks and the timing of the caudal blocks were factors that affected the postoperative pain scores.
In conclusion, a splash block is a simple procedure that produces analgesia with virtually no side-effects when local anesthetics are instilled into the incision site, and the local anesthetics are absorbed into the muscular coat and exposed nerves. Unlike caudal blocks, this analgesic method does not require advanced anatomical knowledge, nor is the procedure difficult. We think a caudal block is an adequate analgesic method for the patients who can not receive a splash block or for those patients who were expected to experience complications after a splash block.
To replace caudal blocks in the future, further research is required using a greater sample size, as well as conducting pain score evaluations from post-surgery to the point of discharge, noting the types and concentrations of the employed local anesthetics, determining the effects of the caudal block performed pre- and post-surgery on the pain scores as compared to that when splash blocks are used, and evaluating the postoperative pain scores in a sample group of patients for whom local anesthetics are not used.