|
 |
|
|
Abstract
Background
Prevention of intraoperative hypothermia has become a standard of operative care. Since ephedrine has a thermogenic effect and it is frequently used to treat hypotension during anesthesia, this study was designed to determine the effect of ephedrine on intraoperative hypothermia of patients who are undergoing spine surgery.
Methods
Twenty-four patients were randomly divided to receive an ephedrine (the ephedrine group, n = 12) or normal saline (the control group, n = 12) infusion for 2 h. The esophageal temperature (the core temperature), the index finger temperature (the peripheral temperature) and the hemodynamic variables such as the mean blood pressure and heart rate were measured every 15 minutes after the intubation.
Results
At the end of the study period, the esophageal temperature and hemodynamic variables were significantly decreased in the control group, whereas those in the ephedrine group were stably maintained. The index finger temperature was significantly lower in the ephedrine group compared to that in the control group, suggesting the prevention of core-to-peripheral redistribution of the heat as the cause of temperature maintenance.
Preventing intraoperative hypothermia has become a standard of care because maintaining the perioperative normothermia is associated with an improved surgical outcome. Hypothermia increases the blood loss by impairing the blood coagulation profile, it prolongs the action of drugs and it increases surgical wound infection [1-4].
Various methods have been introduced to maintain normothermia during general anesthesia. A warm mattress and a forced air warming device are most commonly used. However, for patients undergoing spine surgery, the warm mattress cannot be used and a forced air warming device has little effect because the body surface that needs to be covered by the device is small. Beside external warming devices, anesthetic agents have been reported to influence intraoperative thermoregulation [5] and the previous studies on intraoperative temperature management have reported the thermogenic effect of an amino acid solution both during general and spinal anesthesia [6,7]. Among the drugs with a known thermogenic effect, ephedrine was frequently used in obese patients for its thermogenic and anti-appetite effect until its adverse effects prevented its use [8].
Ephedrine is frequently used to treat hypotension during anesthesia, but there has been no report on the intraoperative thermogenic effect of ephedrine. Therefore, this study was designed to determine the effect of ephedrine on the intraoperative hypothermia of patients who are undergoing spine surgery.
This study was approved by the Institutional Review Board and informed consent was obtained from all the patients. Twenty-four patients of American society of anesthesiologist class I or II were included in this study. The patients with a history of thyroid disease, dysautonomia or fever within a week before surgery, or those who were obese (a body mass index > 35) were excluded from this study. The patients were randomly divided into the ephedrine group (n = 12) and the control group (n = 12) using a computer generated randomization list in a sealed envelope. The study drug was mixed in a 50 ml syringe by an independent researcher in the following concentrations: ephedrine 1 mg/ml and normal saline.
The surgeries were performed between 8 : 00 am and 12 : 00 am to avoid diurnal variation. The ambient operating room (OR) temperature was maintained around 20 degrees Celsius (Ōäā). On arrival in the OR, standard anesthetic monitors were applied, including ECG, a non-invasive blood pressure monitor and pulse oximetry. The skin temperature probe was attached on the index finger of the non-infused arm. Anesthesia was induced with propofol 1.5 mg/kg and remifentanil 1 ug/kg. The endotracheal intubation was facilitated with rocuronium 0.6 mg/kg. The patients were mechanically ventilated with 60% inspired oxygen with air to maintain the end-tidal carbon dioxide between 35-40 mmHg. The anesthesia was maintained with an end-tidal concentration of sevoflurane 1 vol% and remifentanil 0.1 ug/kg/min. An esophageal temperature probe was inserted into the lower esophagus immediately after the intubation for measuring the core temperature. Five min after the intubation, the study drug was started at a rate of 50 ml/h (ephedrine 50 mg/h) for 2 min and then at 10 ml/h (ephedrine 10 mg/h) for next 113 min with using a syringe pump. The patients with tachycardia (a heart rate [HR] > 100 beat/min) or hypertension (a systolic blood pressure [SBP] 20% higher than the baseline or higher than 140 mmHg) were dropped from the study. When the SBP fell 20% below the baseline or lower than 90 mmHg, phenylephrine 100 ug was given at 2 min intervals. If the hypotension persisted after 2 consecutive bolus doses of phenylephrine, then the dose of remifentanil was reduced to 0.05 ug/kg/min. Lactate Ringer's solution was infused at a constant rate of 6 ml/kg/h. Six percent hydroxyethyl starch (Voluven, Fresinius Kabi, Bad Homberg, Germany) was infused when the blood loss was more than 500 ml. The fluid temperature was maintained at room temperature. The position was changed to the prone position between T10 and T25. After 120 min, the patients with an esophageal temperature below 35Ōäā were warmed with a Bair Hugger forced air warmer (Augustine Medical Inc., Minnesota, USA).
The skin temperature, the SBP, the mean blood pressure (MBP) and the HR were recorded before anesthesia induction (Tpreop), immediately after (Tintu), 10 min after the start of ephedrine infusion (T10) and at 15 min interval (T10-T115) afterwards. The esophageal temperature was measured at Tintu-T115. The room temperature, the fluid intake, the need for and amount of transfusion, the urine output and the blood loss at T115 were recorded.
The sample size was calculated based on a previous study [9]. The mean difference and standard deviation of 0.4 and 0.3Ōäā, respectively, with an alpha error of 0.5 and power of 80% resulted in 10 patients in each group, and a drop out rate of 20% was added.
The statistical analysis was performed with SAS 9.1.3 (SAS Institute, Cary, NC). The data is expressed as the number of patients or means ┬▒ SDs. Comparisons of the continuous data within the groups, such as temperature and the hemodynamic variables, were performed with repeated measures of ANOVA followed by paired t-tests with Bonferroni correction for multiple comparisons. Student's t-test or chi-square tests were used to compare variables between the groups where appropriate.
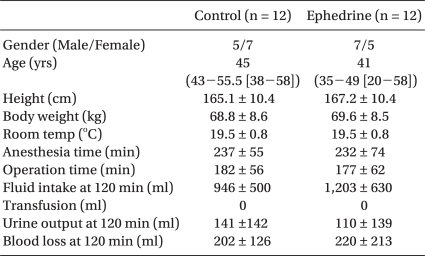
The patient characteristics and perioperative data are listed in Table 1. There was no statistical difference in the patient characteristics and the perioperative data, including the room temperature, fluid intake, blood loss and urine output. None of the patients received a transfusion.
The esophageal temperature at T100 and T115 was significantly decreased from Tintu in the control group (Fig. 1). The esophageal temperature in the ephedrine group was stably maintained. From T55 until the end of study period (T115), the index finger temperature in the ephedrine group was significantly decreased compared to that at Tintu (Fig. 1). In the control group, the index finger temperature at T115 was lower than that at Tintu.
The MBP and HR were stably maintained in the ephedrine group (Fig. 2). In the control group, the MBP and HR were significantly decreased from Tpreop throughout the study period, except at Tintu and T25. The MAP was decreased 20% below baseline in 2 patients in the control group and a phenylephrine bolus was administered to both of them. The MAP was maintained within 20% of baseline in all the patients of the ephedrine group.
This study demonstrated that an infusion of ephedrine prevented the decrease of the core temperature during spine surgery with the patient under general anesthesia. In addition, the MAP and HR were stably maintained throughout the study period.
Ephedrine mediates its thermogenic effects primarily by enhancing the sympathetic neuronal release of norepinephrine and epinephrine, which stimulates directly brown adipocyte respiration via the beta-adrenoreceptors [10-12]. Tolerance to the pressor effects develops rapidly, but tolerance to the thermogenic effects does not, which may suggest the involvement of different adrenoreceptors [13]. The thermogenesis of ketamine and an amino acid infusion has previously been studied during anesthesia and the authors reported its effectiveness for preventing hypothermia during both spinal and general anesthesia [6,7,9,14]. In this study, although it was not statistically significant, the mean core temperature in the ephedrine group increased 0.1Ōäā whereas that in the control group decreased 0.23Ōäā. Therefore, the maintenance of the core temperature in the ephedrine group can be explained in part by the thermogenic effect of ephedrine.
Flynn et al. [15] reported successful treatment of cyclic hypothermia with ephedrine. The patient with cyclic hypothermia had a low thermoregulatory set point and therefore the patient manifested with inappropriate vasodilation and failure to shiver unless cooled further, which is similar to an anesthetized condition. After anesthesia induction, the core hypothermia (0.5-1.5Ōäā) is largely caused by an internal core-to-peripheral redistribution of the body heat due to anesthesia-induced vasodilation and the reduced thermoregulatory vasoconstriction. The effects of anesthesia induction are due to the effect of the anesthetic agents. Propofol, sevoflurane and remifentanil were used in this study. Although propofol was reported to cause more severe hypothermia than sevoflurane by inhibiting thermoregulatory vasoconstriction, Im et al. [16] reported no difference of the core temperature between the two agents. In addition, remifentail was reported to be associated with an increased incidence of post-anesthetic shivering, but it is not a phenomenon of intraoperative hypothermia and it is more likely the result of acute opioid tolerance and stimulation of the N-methyl-D-aspartate receptor [17]. In this study, the index finger temperature was significantly decreased whereas the core temperature was nearly constantly maintained. The vasoconstriction effect of ephedrine may have prevented the internal core-to-peripheral redistribution of heat. This is likely since the significant decrease in the index finger temperature in the ephedrine group started at T55, whereas the decrease in the control group was significant at T115. Therefore, ephedrine was effective in maintaining the core temperature through a thermogenic effect as well as due to the inhibition of redistribution via peripheral vasoconstriction.
The temperature was measured for 2 hrs in this study because a rapid decrease in the core temperature, by about 1-1.5Ōäā, occurs during the first hour of anesthesia. This is followed by a slower, nearly linear decrease of the core temperature, which eventually reaches a plateau [18]. The dose of ephedrine in this study was based on a study by Gajraj et al. [19], in which the prophylactic infusion of ephedrine prevented hypotension dur ing spinal anesthesia without incur r ing reactive hypertension. Intraoperative fluctuation of the blood pressure is frequent and this may lead to serious complications, and especially in elderly patients. In this study, the MAP and HR in the ephedrine group were stably maintained, whereas those in the control group were significantly decreased as compared to the baseline values.
One of the limitations of this study is the lack of the preoperative esophageal temperature. An esophageal temperature probe was not inserted before anesthesia induction because of consideration for the patient's comfort. Another limitation is the use of phenylephrine in 2 patients in the control group. Since phenylephrine is a vasoconstrictor, it may have affected the heat redistribution. However, since the index finger temperature was constantly maintained, this would not have affected the results of this study.
In conclusion, an intraoperative infusion of ephedrine minimized the decrease of the core temperature and it stably maintained the hemodynamic variables during spine surgery with the patients under general anesthesia.
References
1. Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology 2008; 108: 71-77. PMID: 18156884.


2. Heier T, Caldwell JE, Sessler DI, Miller RD. Mild operative hypothermia increases duration of action and spontaneous recovery of vecuronium blockade during nitrous oxide-isoflurane anesthesia in humans. Anesthesiology 1991; 74: 815-819. PMID: 1673591.


3. Carli F, Emery PW, Freemantle CAJ. Effect of preoperative normothermia on postoperative protein metabolism in elderly patients undergoing hip arthroplasty. Br J Anaesth 1989; 63: 276-282. PMID: 2803885.



4. Sessler DI, Rubenstein EH, Moayeri A. Physiological responses to mild perianesthetic hypothermia in humans. Anesthesiology 1991; 75: 594-610. PMID: 1928769.


5. Goto T, Matsukawa T, Sessler DI, Uezono S, Ishiguro Y, Ozaki M, et al. Thermoregulatory thresholds for vasoconstriction in patients anesthetized with various 1-minimum alveolar concentration combinations of xenon, nitrous oxide, and isoflurane. Anesthesiology 1999; 91: 626-632. PMID: 10485770.


6. Kasai T, Nakajima Y, Matsukawa T, Ueno H, Sunaguchi M, Mizobe T. Effect of preoperative amino acid infusion on thermoregulatory response during spinal anaesthesia. Br J Anaesth 2003; 90: 58-61. PMID: 12488380.



7. Sahin A, Aypar U. Effect of amino acid solutions on intraoperative hypothermia and postoperative shivering. Comparison of two anesthetic regimens. Acta Anaesthesiol Scand 2002; 46: 64-67. PMID: 11903074.


8. Diepvens K, Westerterp KR, Westerterp-Plantenga MS. Obesity and thermogensis related to the consumption of caffeine, ephedrine, capsaicin, and green tea. Am J Physiol Regul Integr Comp Physiol 2007; 292: R77-R85. PMID: 16840650.


9. Kinoshita T, Suzuki M, Shimada Y, Ogawa R. Effect of low-dose ketamine on redistribution hypothermia during spinal anesthesia sedated by propofol. J Nippon Med Sch 2004; 71: 92-98. PMID: 15260082.


10. Dulloo AG. Ephedrine, xanthhines and prostaglandin-inhibitors: actions and interactions in the stimulation of thermogenesis. Int J Obes Relat Metab Disord 1993; 17: S35-S40. PMID: 8384178.

11. Dulloo AG, Seydoux J, Girardier L. Potentiation of the thermogenic antiobesity effects of ephedrine by dietary methylxanthines: adenosine antagonism or phosphodiesterase inhibition. Metabolism 1992; 41: 1233-1241. PMID: 1435297.


12. Bukowiecki L, Jahjah L, Follea N. Ephedrine, a potential slimming drug, directly stimulates thermogenesis in brown adipocytes via beta-adrenoreceptors. Int J Obes 1982; 6: 343-350. PMID: 6290407.

13. Dulloo AG, Seydoux J, Girardier L. Peripheral mechanisms of thermogenesis induced by ephedrine and caffeine in brown adipose tissue. Int J Obes 1991; 15: 317-326. PMID: 1885257.

14. Kamitani K, Higuchi A, Nohara A, Takagi M, Tokutake M, Horikawa H, et al. Effect of amino acid solution on intraoperative core temperature the influence of anesthetics. Masui 2005; 54: 1258-1262. PMID: 16296364.

15. Flynn MD, Sandeman DD, Mawson DM, Shore AC, Tooke JE. Cylclical hypothermia: successful treatment with ephedrine. J R Soc Med 1991; 84: 752-753. PMID: 1774760.



16. Im UJ, Lee DJ, Kim MC, Lee JS, Lee SJ. Difference in Core temperature in response to propofol-remifentanil anesthesia and sevoflurane-remifentanil anesthesia. Korean J Anesthesiol 2009; 57: 704-708.


17. Nakasuji M, Nakamura M, Imanaka N, Tanaka M, Nomura M, Suh SH. Intraoperative high-dose remifentanil increases post-anaesthetic shivering. Br J Anaesth 2010; 105: 162-167. PMID: 20542888.



18. Muldoon S, Sambuughin N, Voelkel M, Bunger R, Grocott H, Sulzer C. Malignant hyperthermia, thermoregulation, and perioperative hypothermia. 2008, 1st ed. China, McGraw-Hill Companies, Inc.. pp 1986-1989.
19. Gajraj NM, Victory RA, Pace NA, Van Elstraete AC, Wallace DH. Comparison of an ephedrine infusion with crystalloid administration for prevention of hypotension during spinal anesthesia. Anesth Analg 1993; 76: 1023-1026. PMID: 8484502.


Fig.┬Ā1
Change in the esophageal and index finger temperatures. The data is expressed as means ┬▒ SEs. Preop: before induction of general anesthesia, Intu: immediately after intubation, T10-115: 10 to 115 minutes after the start of ephedrine infusion. *P < 0.05 compared to the
value at Tintu.

- TOOLS