 |
 |
| Korean J Anesthesiol > Volume 75(5); 2022 > Article |
|
Abstract
Background
Of the three common central access sites, subclavian vein catheterization has the lowest risk of infection but the highest risk of pneumothorax. The main disadvantage of the short-axis ultrasound guided approach is difficult needle-tip visualization. We describe use of the hydrolocation technique to improve needle-tip localization.
Case
Two females, an 81-year-old and a 72-year-old, presented for coronary artery bypass grafting requiring central vein cannulation. To confirm that the needle tip was visualized and not the shaft, needle advancement was paused and 1 ml of saline injected. The appearance of a small anechoic pocket superficial to the subclavian vein helped to visualize the needle tip. Negative aspiration was then re-applied and slight advancement resulted in aspiration of blood and successful subclavian vein puncture.
Central venous cannulation is a common procedure in the operating room and critical care settings. Of the three common central access sites, subclavian vein catheterization has the lowest risk of infection and symptomatic thrombosis but the highest risk of pneumothorax [1]. Compared to the traditional landmark technique for subclavian vein access, the use of ultrasound guidance reduces adverse events such as inadvertent arterial puncture, hematoma formation, and pneumothorax [2,3]. When performing ultrasound-guided subclavian vein catheterization, utilizing a short-axis approach has a greater overall success rate, shorter insertion time, and fewer complications as compared to a long-axis approach [3].
The main disadvantage of the short-axis approach is difficult needle tip visualization, with its location often inferred by the movements of surrounding tissues [3]. Even when the hyperechoic needle is visualized, the shaft may be mistaken for the tip. Within the regional anesthesia literature, the technique of hydrolocation is suggested to aid needle tip identification. It is described as ‘the rapid injection of a small amount of fluid (0.5–1 ml) to confirm needle-tip position by both tissue movement and the appearance of a small anechoic “pocket”’ [4]. We therefore describe use of the hydrolocation technique during ultrasound-guided short-axis subclavian vein access to improve needle-tip localization in this mini-case series.
Two female patients, an 81-year-old with body mass index (BMI) 24 kg/m2 and a 72-year-old with BMI 35 kg/m2 presented for coronary artery bypass grafting requiring central vein cannulation. Written informed consent for case reports publication was obtained from both patients. Under general anesthetic and positive pressure ventilation, the patients were placed in 20 degrees Trendelenburg and prepped for left subclavian vein access. During tray set-up, the 18 g, 6.35 cm introducer needle was attached to the 5 ml introduction syringe, and 3 ml of sterile normal saline was drawn up through the needle. This ensured the introducer needle was primed with normal saline and not air, which would obscure the ultrasound image during hydrolocation. The linear ultrasound probe (4.2–13.0 MHz) (LOGIQ™ E ultrasound, GE Healthcare, USA) was placed in the lateral sub-clavicular region and the subclavian vein and artery identified in short-axis. The vein was followed medially until the clavicle was just visible at the cephalad edge of the ultrasound image and the vein was immediately caudad to the clavicle. After skin puncture, negative aspiration was applied to the saline loaded syringe/needle as it was advanced into the deeper subcutaneous structures.
In the first case, the needle can be seen in Fig. 1A (Supplementary Video 1), superficial to the subclavian vein. To confirm this was indeed the needle tip and not the shaft, needle advancement was paused and 1 ml of saline injected. The appearance of a small anechoic pocket superficial to the subclavian vein helped to confirm needle tip position as seen in Fig. 1B (Supplementary Video 1).
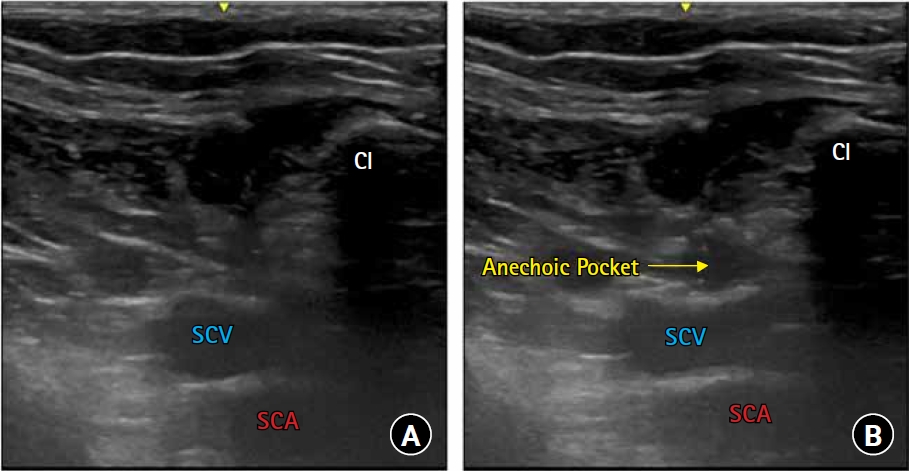
In the second case, difficulty was encountered visualizing the needle and the needle tip was approximated using controlled gentle micro movements and observing for corresponding surrounding tissue movement prior to the 1 ml saline injection as seen in Fig. 2A. The appearance of a small anechoic pocket superficial to the subclavian vein helped to better approximate needle tip position as seen in Fig. 2B (Supplementary Video 2). The subclavian vein also becomes more ovoid as the injection compresses it slightly. Negative aspiration was then re-applied and slight advancement resulted in aspiration of blood and successful subclavian vein puncture. The Seldinger technique and a percutaneous sheath introducer kit (ARROW® PSI, Teleflex Medical, USA) was then used to successfully place a side-port with a single lumen introducer catheter.
The use of hydrolocation for subclavian venous access was easily implemented, required little modification in setup and technique, and provided improved localization of the needle tip. Kim et al. [5] recently published a randomized non-inferiority trail investigating the incidence of catheterization-related complications between supra- and infraclavicular ultrasound-guided subclavian venous catheterization approaches. The reported statistically non-significant but potentially clinically significant difference in pneumothorax cases, two in the infraclavicular and none in the supraclavicular approach, was ‘thought to be due to the difference in ability to view and identify the needle tip despite the use of ultrasound’ [5]. Conceivably, the hydrolocation technique could potentially reduce complications such as pneumothorax, but further research would be required to verify this. We encountered difficulty visualizing the needle in case 2 likely secondary to increased BMI making the ultrasound views more difficult. In this case, the use of hydrolocation was regarded as being even more useful in approximating needle tip position as compared to case 1 where hydrolocation was used more as a confirmation of needle tip location. Without the use of hydrolocation in case 2, the next confirmatory endpoints would be aspiration of blood (indicating arterial or venous puncture) or air (indicating pleural puncture and pneumothorax). The hydrolocation technique provided reassurance that even when the needle is difficult to visualize (case 2) the needle tip is still above the puncture site of interest and not approaching the pleura.
A 1 ml injection was used, representing the upper limit of optimal injection volume (0.5–1 ml), as recommended in the regional literature describing the hydrolocation technique [4]. Though an increased injection volume may help to better visualize the forming anechoic pocket on ultrasound, it has the potential to further distort the anatomy and introduce air bubbles creating a suboptimal ultrasound image. We recognize the possibility that the appearance of the anechoic pocket may be misaligned with the needle tip secondary to fluid tracking proximally or distally to the needle. Nonetheless, the hydrolocation technique provides additional information on approximating the needle tip position allowing for a more confident approach to central access. We stress the importance of introducer needle priming with normal saline to prevent air injection and subsequent ultrasound image artifact.
This case series is a preliminary report of a novel approach to central venous catheterization using hydrolocation. However, we are unable to demonstrate that the technique of hydrolocation during ultrasound guided central line placement provides added safety compared to conventional methods given insufficient number of patients, lack of a comparison group, and lack of statistical evidence. Therefore, no definitive recommendations are made. However, the described technique of hydrolocation offers proof of concept and preliminary data for ongoing investigation into this novel technique. Although we describe the approach for subclavian venous access, the hydrolocation technique could easily be applied to alternative central access sites.
Fig. 1.
Hydrolocation to confirm needle tip location (A) Short-axis view: Needle positioned midline and superficial to subclavian vein. (B) Confirming needle tip location: 1 ml of normal saline was injected and an anechoic pocket is seen being formed superficial to the subclavian vein. Cl: clavicle, SCV: subclavian vein, SCA: subclavian artery.
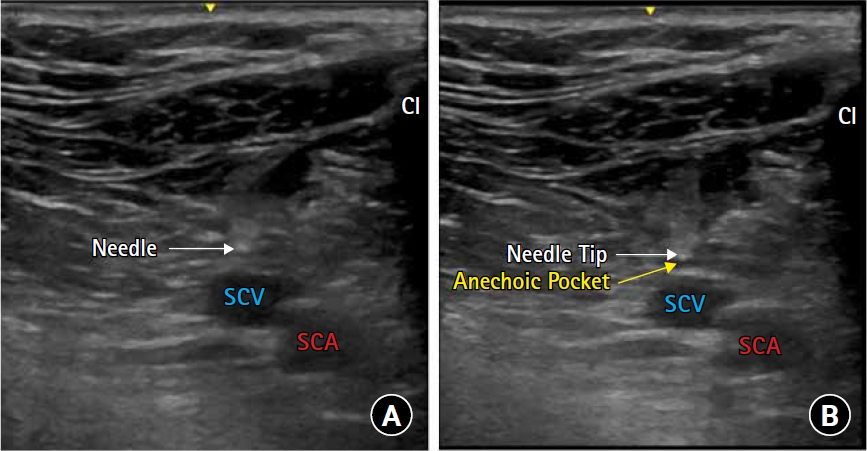
Fig. 2.
Hydrolocation to localize needle tip (A) Short-axis view: Difficult needle tip position approximation. (B) Localizing needle tip location: 1 ml of normal saline was injected and an anechoic pocket is seen being formed superficial to the subclavian vein. Cl: clavicle, SCV: subclavian vein, SCA: subclavian artery.
References
1. Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, et al. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med 2015; 373: 1220-9.


2. Lalu MM, Fayad A, Ahmed O, Bryson GL, Fergusson DA, Barron CC, et al. Ultrasound-guided subclavian vein catheterization: a systematic review and meta-analysis. Crit Care Med 2015; 43: 1498-507.


3. Vezzani A, Manca T, Brusasco C, Santori G, Cantadori L, Ramelli A, et al. A randomized clinical trial of ultrasound-guided infra-clavicular cannulation of the subclavian vein in cardiac surgical patients: short-axis versus long-axis approach. Intensive Care Med 2017; 43: 1594-601.












